Ad
Skin cancer
Application to facilitate skin self-examination and early detection. read more.
What is it cutaneous scaly cell carcinoma?
Cutaneous squamous cell carcinoma (SCC) is a common type of keratinocytes Canceror notmelanoma skin cancer. It is derived from cells within the epidermis that does curb – the horny protein that forms the skin, hair and nail.
Cutaneous SCC is a invader disease, which refers to cancer cells that have grown beyond the epidermis. SCC can sometimes metastasis and it can be fatal
Intraepidermal carcinoma (SCC cutaneous in the place) and mucous membrane SCC are considered elsewhere.
Who gets cutaneous squamous cell carcinoma?
Risk factors for cutaneous SCC include:
- age and sex: CECs are particularly predominant in older men. However, they also affect women and younger adults.
- Previous SCC or another form of skin cancer (basal cell carcinoma, melanoma) are a strong predictor of future skin cancers.
- Actinic keratosis
- Outdoor occupation or recreation
- Of smoking
- Fair skin, blue eyes, and blonde or red hair.
- Previous skin injury, thermal burn, disease (eg, cutaneous lupus, epidermolysis bullosa, leg ulcer)
- Hereditary syndromes: SCC is a particular problem for families with xeroderma pigmentosum and albinism.
- Other risk factors include ionizing radiation, exposure to arsenic, and immunosuppression due to illness (eg. chronic lymphocytic leukemia) or medications. Organ transplant Recipients are at massive risk of developing SCC.
What Causes Cutaneous Squamous Cell Carcinoma?
More than 90% of SCC cases are associated with numerous DNA mutations in multiple somatic genes. Mutations in p53 tumor suppressor gene are caused by exposure to Ultraviolet radiation (UV), especially UVB (known as signature 7). Other characteristic mutations are related to smoking, aging, and immune suppression (for example, with drugs such as azathioprine). Mutations in signaling pathways affect epidermal growth factor receiver, RAS, Fyn and p16INK4a signaling.
Beta-genus human papillomaviruses (wart viruses) are thought to play a role in SCC arising in immunocompromised populations. β-HPV and HPV 5, 8, 17, 20, 24, and 38 subtypes have also been associated with an increased risk of cutaneous SCC in immunocompetent individuals.
What are the clinical features of cutaneous squamous cell carcinoma?
Cutaneous SCC present as enlargement scaly or crusty lumps. They usually arise within pre-existing actinic keratosis or intraepidermal carcinoma.
- They grow for weeks or months.
- They can ulcerate
- They are often tender or painful.
- Located on sun-exposed sites, particularly the face, lips, ears, hands, forearms, and legs
- The size varies from a few millimeters to several centimeters in diameter.
Squamous cell carcinoma of the skin

Squamous cell carcinoma

Squamous cell carcinoma

Squamous cell carcinoma
See more images of squamous cell carcinoma:
- SCC on the face
- SCC on the lip
- SCC in the ear
-
SCC in the extremities.
Types of cutaneous squamous cell carcinoma
The different clinical types of invasive cutaneous SCC include:
-
Cutaneous horn – the horn is due to excessive production of keratin
-
Keratoacanthoma (KA): a rapidly growing keratinization nodule that can be resolved without treatment
-
Carcinoma cuniculatum ('warty carcinoma”), a slow growth, warty tumor on the sole of the foot.
- Multiple SCC/KA type eruptive lesions arising in syndromes such as multiple self-healing squamous epitheliomas by Ferguson-Smith and Grzybowski syndrome
the pathologist can also classify a tumor differentiated, moderately well differentiated, poorly differentiated, or anaplastic Cutaneous SCC. There are other variants.
Subtypes of Cutaneous Squamous Cell Carcinoma
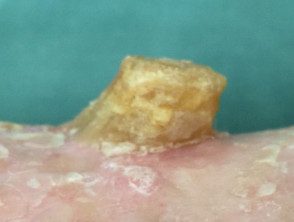
Cutaneous horn

Keratoacanthoma

Cuniculatum carcinoma

Ferguson-Smith squamous epithelioma

Grzybowski syndrome
Classification of squamous cell carcinoma by risk
Cutaneous SCC is classified as low risk or high risk, depending on the possibility of tumor reappearance and metastasis. Features of high-risk SCC include:
High-risk cutaneous squamous cell carcinoma has the following characteristics:
- Diameter greater than or equal to 2 cm.
- Location in the ear, lip vermilion, central face, hands, feet, genitalia.
- In elderly or immunocompromised patients.
- Histological thickness greater than 2 mm, poorly differentiated histologyor with the invasion of subcutaneous tissue, nerves and blood vessels
Metastatic SCC is located in regional lymph nodes (80%), lungs, liver, brain, bones and skin.
High-risk cutaneous squamous cell carcinoma.

High-risk cutaneous squamous cell carcinoma.

High-risk cutaneous squamous cell carcinoma.

High-risk cutaneous squamous cell carcinoma.
Cutaneous squamous cell carcinoma staging
In 2011, the American Joint Committee on Cancer (AJCC) published a new staging systemic for Cutaneous SCC for the AJCC Manual 7th Edition. This evaluates the dimensions of the original. primary tumor (T) and its metastasis to the lymph nodes (N).
Tumor staging for cutaneous SCC
TX: primary tumor cannot be assessed
T0: no evidence of a primary tumor
Tis: carcinoma in situ
T1: Tumor ≤ 2 cm without high-risk features
T2: tumor ≥ 2 cm; either; Tumor ≤ 2 cm with high-risk features
T3: tumor with invasion of the maxilla, mandible, orbit or temporary bone
T4: tumor with invasion of axial or appendicular skeleton or perineural skull base invasion
Nodal staging of cutaneous SCC
NX: regional lymph nodes cannot be assessed
N0: non-regional lymph node metastasis
N1: metastasis in a local lymph node ≤ 3 cm
N2: metastasis in a local lymph node ≥ 3 cm; either; Metastasis in > 1 local lymph node ≤ 6 cm
N3: lymph node metastasis ≥ 6 cm
How is squamous cell carcinoma diagnosed?
The diagnosis of cutaneous SCC is based on clinical features. The diagnosis and histological subtype are confirmed pathologically by diagnosis. biopsy or following excision. See squamous cell carcinoma – pathology.
High-risk SCC patients may also undergo staged investigations to determine if it has spread to the lymph nodes or elsewhere. These may include:
- images using ultrasound scan, x-ray, Connecticut scans, Magnetic resonance scans
- lymph node or other tissue biopsies
What is the treatment for cutaneous squamous cell carcinoma?
Cutaneous SCC is almost always treated surgically. Most cases are removed with a 3- to 10-mm margin of normal tissue around a visible tumor. A flap or skin graft may be needed to repair the defect.
Other removal methods include:
- Shaving, curettage and electrocautery for low-risk trunk and extremity tumors
- Aggressive cryotherapy for very small, thin, low-risk tumors
-
Mohs micrographic surgery for large facial lesions with indistinct margins or recurrent tumors
- Radiotherapy for an inoperable tumor, patients unfit for surgery, or as assistant
What is the treatment for advanced or metastatic squamous cell carcinoma?
Locally advanced primary, recurrent, or metastatic SCC requires multidisciplinary consultation. A combination of treatments is often used.
- Surgery
- Radiotherapy
- Cemiplimab
- Experimental targeted therapy using epidermal growth factor receptor inhibitors
Many thousands of New Zealanders are treated for cutaneous SCC each year, and more than 100 die from their disease.
How can cutaneous squamous cell carcinoma be prevented?
There is a large body of evidence showing that very careful sun protection at any time in life reduces the number of SCC. This is particularly important on aged, sun-damaged, fair skin; in immunocompromised patients; and in those who already have previous actinic keratoses or SCCs.
- Staying indoors or in the shade in the middle of the day.
- Wear clothing that covers
- Generously apply broad-spectrum sunscreens with protection factor SPF50+ to exposed skin yes outside
- Avoid tanning indoors (hammocks, solaria)
Oral nicotinamide (vitamin B3) at a dose of 500 mg twice daily may reduce the number and severity of SCCs in people at high risk.
Patients with multiple squamous cell carcinomas may be prescribed an oral medication. retinoid (acitretin or isotretinoin). These reduce the number of tumors but have some troublesome side effects.
What is the prognosis for cutaneous squamous cell carcinoma?
Most SCCs are cured by treatment. A cure is more likely if treatment is carried out when the injury it is small. The risk of disease-associated recurrence or death is greater for tumors that are >20 mm in diameter and/or >2 mm thick at the time of surgical excision.
About 50% of people at high risk for SCC develop a second one within 5 years of the first. They are also at increased risk of other skin cancers, especially melanoma. Periodic skin exams and annual long-term skin checks by an experienced healthcare professional are recommended.


