What is it urticaria?
Urticaria is a condition characterized by the presence of cure (hives) and angioedema [1,2].
- A bump It is a superficial swelling of red or pale skin, usually surrounded by erythema, which can persist from a few minutes to 24 hours. Hives are usually very itchy, but they can also cause a burning sensation.
- Angioedema is deep swelling. dermal layers of skin or mucous membranes Swelling is usually skin-colored, but may be erythematous. Angioedema can be asymptomatic, itchy or causes burning pain. It may take up to 72 hours to resolve.
Scarring is accompanied by angioedema in up to 40% cases, but angioedema may occur only in some people. [2].
Hives affect one in four people at some point in their lives. [3] and can be classified by duration, acute or chronicand for reasons, whether spontaneous or inducible [1,2]. Two or more different subtypes of urticaria can coexist in a person [1,2].
Acute urticaria is the daily or episodic occurrence of scarring, angioedema, or both, for less than 6 weeks. [1,2]. There are multiple possible causes, including infections or allergies, but it is often idiopathic [2].
Figure 1. Classification of urticaria.
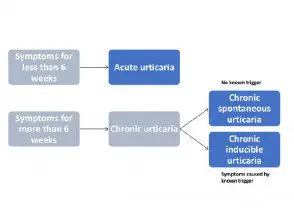
Classification of urticaria
Adapted from Zuberbier T et al, 2018.
Spontaneous urticaria and angioedema

Spontaneous urticaria

Spontaneous urticaria

What is chronic urticaria?
Chronic urticaria is the daily or episodic appearance of scarring, angioedema, or both, for 6 weeks or more. [1,2]. Chronic hives may persist for 1 to 5 years, sometimes longer. [2,4].
International guidelines for the classification, diagnosis and treatment of chronic urticaria have recently been published based on a consensus of multiple national and international societies. [1].
Chronic urticaria can be classified as spontaneous or inducible, and both types can coexist in a patient [1,2]. This article is about chronic spontaneous urticaria. (See DermNet NZ page on chronic inducible urticaria.)
What is spontaneous chronic urticaria?
Chronic spontaneous urticaria refers to chronic hives that do not have a specific cause or trigger. Scars are present most days of the week for 6 weeks or more. [1,2].
Chronic spontaneous urticaria was previously called chronic idiopathic urticaria. This term is no longer used since many cases have a autoimmune base [2].
Who gets chronic hives?
Estimates of the incidence of chronic urticaria varies from 0.05% to 2% of the population in the USA, and up to 20% of the population in Thailand [5].
- Life predominance of chronic urticaria is approximately 1.8% [2].
- Chronic spontaneous urticaria occurs in 0.5 to 1% of the population at any time [3,4].
- Two out of three cases of chronic urticaria are spontaneous, with a maximum incidence between 20 and 40 years of age. [3].
- Most studies have reported that women experience urticaria and chronic urticaria almost twice as often as men [2–4].
- The incidence of urticaria in children has been reported between 2% and 7% [6] and the incidence of chronic urticaria in this age group is between 0.1% and 3% [7].
- Chronic hives are more common in older children and adolescents. [2].
- Spontaneous urticaria is the most common subgroup of chronic urticaria in children. [2].
What are the clinical characteristics of chronic spontaneous urticaria?
Chronic spontaneous urticaria is characterized by the presence of scars and angioedema. [1,2].
Scars can affect any site on the body and tend to be widely distributed [2,8].
- Cracks can be a few millimeters or several centimeters in diameter.
- They can be white or red, usually with a red flash.
- Each healing can last a few minutes or several hours, and they may change shape before resolving.
- Scars can be round or ring-shaped, a map-like pattern, or giant patches.
Hives Riches

Spontaneous urticaria

Spontaneous urticaria

Spontaneous urticaria
See more images of hives and angioedema.
Angioedema is more common. located [8].
- It commonly affects the face (presents as swollen lips or eyelids), hands, feet and genitals.
- It can affect the tongue, uvula, soft palate and pharynx.
Angioedema



Chronic spontaneous urticaria is unpredictable and debilitating. Scars are more persistent in chronic spontaneous urticaria than in chronic inducible urticaria, but each tends to resolve or alter within 24 hours. They can occur at certain times of the day.
Some patients with chronic spontaneous urticaria report that they are associated systemic Symptoms These may include:
- Headache and fatigue.
- Joint pain and inflammation
- Wheezing, redness and palpitations.
- Gastrointestinal symptoms [9].
What is the activity like and control of urticaria evaluated?
There are several validated systems to evaluate urticaria activity and control.
Disease activity in chronic spontaneous urticaria can be assessed with the 7-day urticaria activity score (UAS7), a simple and validated scoring system based on the evaluation of key signs and symptoms of urticaria: pruritus – that are documented by the patient. Daily healing and pruritus scores are summed over 7 days; the maximum score is 42 [1].
| Punctuation | Weals | Punctuation | Pruritus |
|---|---|---|---|
| 0 0 | None | 0 0 | None |
| 1 | Mild (<20 curas> | 1 | Mild (present but not bothersome or problematic) |
| 2 | Moderate (20–50 cures / 24 hours) | 2 | Moderate (problematic but does not interfere with normal daily activity or sleep) |
| 3 | Intense (> 50 weals / 24 hours or large confluent wealth area) | 3 | Severe (severe itching that is problematic enough to interfere with normal daily activity or sleep) |
| Scar score + itch score = daily score. Repeat daily for 7 days and add scores for UAS7. | |||
The urticaria control test (UCT) [10] is useful in the evaluation of the patient's disease status and is validated to determine the level of disease control in both spontaneous chronic urticaria and inducible chronic urticaria [10]. 1]. The UCT has four elements with a clear boundary for “well-controlled” versus “poorly controlled” disease, making it useful in routine clinical practice.
The Angioedema Activity Score (AAS) [11] allows the patient to rate each of the five key factors related to their experience of angioedema from 0 to 3 (giving a daily score of 0-15). The daily AAS can be summed to provide 7-day (AAS7), 4-week (AAS28), and 12-week (AAS84) scores [11].
Assessment of quality of life in chronic urticaria.
Current international guidelines recommend validated instruments to assess the emotional impact of chronic urticaria and the effect on patient quality of life, such as the Chronic Urticaria Quality of Life Questionnaire (CU-Q).2oL) [12] and the Angioedema Quality of Life Questionnaire (AE-QoL) [1,13].
What causes chronic spontaneous urticaria?
Hives are a mast cells-measure of illness. Activated mast cells launching histamine together with other mediators, such as plateletactivation factor and cytokines, resulting in sensory nerve activation, vasodilation, plasma extravasationand recruitment of cells to urticarial injury. many different molecules may activate mast cells in urticaria, but in general, these are not well defined [1].
By definition, chronic spontaneous urticaria has no known trigger. Causes include:
- Autoimmunity mediated by functional autoantibodies against high affinity immunoglobulin E (IgE) receiver
- IgE autoantibodies for autoantigens
- Not-allergic reactions food or drug-induced hives (pseudoallergy)
- Acute or chronic infections as a result of Helicobacter pyloristreptococcus, staphylococcus Yersinia, Giardia lamblia, Mycoplasma pneumoniae, hepatitis viruses, norovirus, parvovirus B19, Anisakis simplex, Entamoeba spp., and Blastocystis spp. [1].
Chronic spontaneous urticaria may be due to type I allergy in exceptionally rare cases [1].
There is a strong association between chronic spontaneous urticaria and other immune disorders, in particular autoimmune thyroid disease. Thyroid autoantibodies are the most common laboratory abnormalities associated with chronic spontaneous urticaria, with most studies reporting elevated levels in 10% or more of affected patients. [2,14]. Thyroid dysfunction Rates also increase in people with chronic spontaneous urticaria, with hypothyroidismand Hashimoto's thyroiditis observed more frequently than hyperthyroidism and Graves' disease [14].
The frequency of underlying causes varies in different studies of chronic spontaneous urticaria, reflecting regional differences in diet or prevalence of infections. [1].
What are the complications of chronic urticaria?
The burden of chronic spontaneous urticaria.
Patients with chronic spontaneous urticaria may experience lack of sleep, anxiety, depression, lack of energy, and social isolation. [fifteen]. This can result in a significant deterioration in the patient's quality of life (see figure 2) [15]. Chronic spontaneous urticaria is unpredictable and can disrupt the patient's normal daily activities.
Figure 2. Impact of chronic spontaneous urticaria on quality of life, sleep and daily activities.
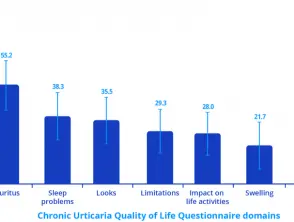
Impact of chronic spontaneous urticaria on quality of life, sleep and daily activities.
Note: A higher score indicates a greater deterioration in quality of life.
Credit: Adapted from Maurer M, et al. Allergy 2017; 72: 2005-16.
How is chronic spontaneous urticaria diagnosed?
Chronic urticaria is diagnosed through a careful history and examination; This diagnosis is based on a history lasting more than 6 weeks of daily or episodic healing lasting less than 24 hours without the presence of physical triggers.
International guidelines provide a diagnostic algorithm for chronic urticaria (see figure 3). The diagnosis of chronic spontaneous urticaria is based on the compilation of a complete medical history that covers:
- Time of onset of the disease.
- The shape, size, frequency and distribution of riches
- Associated angioedema
- Associated symptoms such as bone/joint pain, feverand abdominal cramps
- Personal and family history of diseases and angioedema.
- Induction by physical agents or exercise.
- Event in relation to the day, weekends, menstrual cycle, vacations and trips abroad.
- Occurrence with food or drugs (non-steroidal anti-steroids).inflammatory drugs [[NSAID], angiotensin conversion enzyme [ACE] inhibitors)
- Occurrence with infections or psychological stress.
- Previous or current allergies, infections, internal/autoimmune diseases, gastrointestinal problems or other disorders.
- The social and occupational history of the patient.
- Recreational activities
- Previous therapy and response to treatment, including dose and duration.
- Previous diagnostic procedures and results.
International guidelines recommend limiting investigations in most patients with chronic spontaneous urticaria to differential blood count and erythrocytes sedimentation rate (ESR) and C-reactive protein (CRP) Other diagnostic measures are based on the patient's history and examination, especially in patients with long-standing and uncontrolled disease.
Figure 3. Diagnostic algorithm for chronic urticaria.
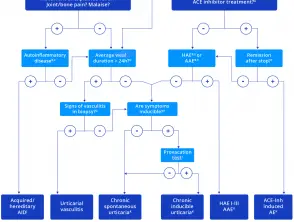
Diagnostic algorithm for chronic urticaria.
Credit: Adapted from Zuberbier T, et al. Allergy 2018.
Notes on the diagnostic algorithm for chronic urticaria
- In addition to ACE inhibitors, other renin inhibitors and sartans have also been reported to induce angioedema, but much less frequently.
- Patients should be asked for a detailed family history and age at onset of illness.
- Test for elevated inflammatory markers (e.g., CRP and ESR), test for paraproteinemia in adults, look for signs of neutrophil-rich infiltrates in skin biopsies, and perform genetic mutation analysis for hereditary periodic fever syndromes (e.g. ., Periodic syndromes associated with cryopyrin) if highly suspected
- Patients should be asked: “How long does each cure last?”
- Test C4 complement and C1 inhibitor levels and function; also test C1q and C1 inhibitory antibodies if angioedema is acquired and suspected; and do genetic mutation analysis if previous tests are unremarkable but the patient's history suggests hereditary angioedema.
- If there is no remission after 6 months of ACE inhibitor discontinuation, test C1 inhibitor levels.
- Does biopsy of lesional skin show damage to small vessels in the papillary and reticular dermis and fibrinoid deposits in perivascular and interstitial locations suggestive of urticarial vasculitis?
- Patients should be asked: “Can you make your scars appear? Can you bring out your riches?
- In patients with a history suggestive of inducible urticaria, standardized provocation tests should be performed according to the international consensus recommendation. [16].
- Acquired autoinflammatory syndromes include Schnitzler syndrome, systemic juvenile idiopathic arthritis, and adult-onset Stills disease; Hereditary autoinflammatory syndrome includes cryopyrin-associated periodic syndromes, such as familial cold autoinflammatory syndrome, Muckle-Wells syndrome, and neonatal-onset multisystem inflammatory disease, more rarely hyper-IgD syndrome and factor receptor-associated periodic syndrome. of tumor necrosis.
- In some rare cases, recurrent angioedema is neither mast cell-mediated nor bradykinin-mediated, and the underlying pathomechanisms remain unknown. Some cases call these rare cases “idiopathic angioedema.”
Which is the differential diagnosis for chronic spontaneous urticaria?
International guidelines recommend that differential diagnoses be considered in all patients with signs or symptoms suggestive of chronic urticaria based on the diagnostic algorithm. These include:
- Autoinflammatory Cryopyrin-associated periodic disorders and syndromes
- Urticaria vasculitis
- Maculopapular cutaneous mastocytosis (urticaria pigmentosa)
- Hereditary angioedema
- ACE inhibitor-induced angioedema
- Schnitzler syndrome
- Gleich syndrome
- Wells syndrome
- Bullous pemphigoid (during the prebullous stage)
-
Induced by exercise anaphylaxis [1].
What is the treatment for chronic hives?
There is no “cure” for chronic hives. The goal of treatment is to achieve symptom-free control [1,2].
The approach to treating chronic spontaneous urticaria may involve:
- Identification and elimination of any underlying causes.
- Avoid any known aggravating factors, such as NSAIDs
- Pharmacological treatment to prevent the release of mast cell mediators or to prevent the effects of mast cell mediators [1].
Often, the treatment of chronic inducible urticaria and chronic spontaneous urticaria will overlap [2].
Elimination of underlying causes.
Chronic spontaneous urticaria is often associated with a variety of inflammatory or infectious diseases. Any identified infectious disease (e.g. H. pylori infection, bacterial infections of the nasopharynxor intestinal parasites) and chronic inflammatory processes (e.g., gastritis, reflux esophagitisand inflammation of the bile duct or gallbladder) must be treated [1].
Plasmapheresis can reduce functional autoantibodies and has been shown to provide temporary benefit in some autoantibodypositive patients with chronic spontaneous urticaria who have not responded to any other form of treatment [1].
Pharmacological treatment of chronic urticaria.
About one-third of patients continue to have symptoms despite maximum tolerated daily doses of non-sedating antihistamine [3].
An algorithm for the symptomatic treatment of chronic urticaria is included in international guidelines (see figure 4) [1]. The algorithm should be used with caution in children with chronic urticaria and in pregnant/nursing women as medications. contraindicated in pregnancy it should not be used [1]. Treatment should be continued until remission occurs.
Figure 4. Pharmacological treatment algorithm.
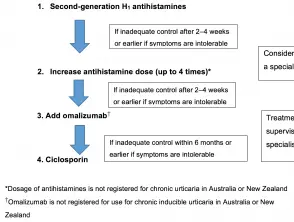
Pharmacological treatment algorithm for chronic urticaria.
Credit: Adapted from Zuberbier T, et al. Allergy 2018.
Antihistamines
Many of the symptoms of urticaria are mediated by the actions of histamine in H1-receptors located in endothelial cells (that cause scars) and sensory nerves (causing neurogenic flare and itching). Continuous treatment with H1-antihistamines is supported by clinical trial data [1,2]. In some forms of physical urticaria, such as cold urticaria, “as needed” treatment may be appropriate [1].
Second-generation antihistamines are recommended in preference to first-generation antihistamines, as these have anticholinergic effects and sedative actions, and interact with alcohol and many drugs that affect the central nervous system. [1]. Second-generation non-sedating antihistamines are the first-line symptomatic treatment for urticaria due to their good safety profiles. [1]. Those studied in the treatment of chronic urticaria include:
- Cetirizine
- Loratadine
- Fexofenadine
- Desloratadine
- Levocetirizine
- Rupatadine
- Bilastine
Terfenadine and astemizole are no longer available in New Zealand or Australia and should not be used as they are cardiotoxic in combination with ketoconazole or erythromycin. [1].
Several small randomized trials have confirmed improvement effectiveness of higher doses of second generation antihistamines up to four times the recommended doses of bilastine, cetirizine, desloratadine, ebastine, fexofenadine, levocetirizine and rupatadine (some of these agents are not available and higher doses are not licensed in New Zealand or Australia ) [1]. Most patients with urticaria who do not respond to standard doses will benefit from antihistamines. [1].
Treatment of refractory chronic spontaneous urticaria
Patients with chronic spontaneous urticaria who have not responded to the maximum dose of second-generation oral antihistamines taken for 4 weeks should be referred to a dermatologist, immunologist or medical allergy specialist [1].
Omalizumab
Omalizumab is completely human. monoclonal antibody which selectively binds to free IgE, reducing the amount of IgE available in the blood and subsequently in the skin [17]. This leads to downregulation of surface IgE receptors, decreasing downstream signaling and resulting in suppressed activation of mast cells and basophils and in reduced inflammatory responses [17].
Omalizumab has been shown to be effective and well tolerated in the treatment of chronic spontaneous urticaria. [18–21]. Phase III studies have demonstrated efficacy at doses of 150 mg to 300 mg every 4 weeks regardless of total serum IgE levels or body weight. Omalizumab improves angioedema [22,23], improves quality of life [22–24], is suitable for long-term use [25], and treats relapse after interruption [26].
The recommended dose for the treatment of chronic spontaneous urticaria is 300 mg per subcutaneous injection every 4 weeks. Some patients may achieve control of their symptoms with a dose of 150 mg every 4 weeks. [17].
Omalizumab is indicated in New Zealand and Australia for adults and adolescents (≥ 12 years of age) with chronic spontaneous urticaria who remain symptomatic despite H1antihistamine treatment [17]. As of August 2018, it is currently listed on the Pharmaceutical Benefits Scheme in Australia for patients with severe chronic spontaneous urticaria, provided specific criteria are met [27]. Omalizumab is funded for use in chronic spontaneous urticaria in New Zealand under Special Authority criteria (see PHARMAC for details) [28].
Cyclosporine
Cyclosporine is a calcineurin inhibitor and has a moderate direct effect on mast cell mediator release. The efficacy of cyclosporine in combination with a second generation H1-antihistamine has been shown in placebocontrolled by the patient in chronic spontaneous urticaria [1]. It is not recommended as standard treatment due to the risk of significant adverse effects. [1]. Cyclosporine should be reserved for patients with severe refractory chronic spontaneous urticaria [1].
Corticosteroids
-
Systemic corticosteroids have not been studied in randomized controlled trials and evidence for their use in chronic urticaria is limited. [1,2].
- Long-term use of systemic corticosteroids should be avoided as high doses are often required to reduce the symptoms of urticaria with the associated potentially serious adverse effects. [1,2].
- A short course of systemic steroids may be considered for severe patients. exacerbations of chronic urticaria [1,2].
Other treatments
Other agents have been used off-label for the treatment of chronic spontaneous urticaria, but have little evidence to support them. These treatments include:
- Leukotrienes receptor antagonists (e.g., montelukast)
- Dapsone
- H2 antagonists (see antihistamines)
- Sulfasalazine
- Methotrexate
- Mycophenolate
- Hydroxychloroquine
- Interferon
- Plasmapheresis
- Phototherapy
-
Intravenous immunoglobulin [1,29].
These treatments may be valuable for individual patients in particular clinical situations.
What is the outcome of chronic spontaneous urticaria?
Chronic spontaneous urticaria has a high remission rate; this remission rate was up to 80% in 12 months in a population study [4]. However, symptoms were reported to last for more than 1 year in up to 20% patients and for more than 5 years in 11,3% patients in another study [2,4].
