What is the drug? hypersensitivity syndrome?
Drug hypersensitivity syndrome is a severe and unexpected reaction to a drug, affecting several organ systems at the same time. It most often causes the combination of:
- High fever
- Morbid eruption
- Hematological abnormalities
- Lymphadenopathy
- Inflammation of one or more internal organs
Drug hypersensitivity syndrome is also sometimes called a drug reaction with eosinophilia and systemic symptoms (DRESS) and drug-induced hypersensitivity syndrome (DIHS).
The syndrome is classified as severe. cutaneous adverse reaction (SCAR). May Have Features Overlapping With Stevens-Johnson Syndrome / toxic epidermal necrolysis (SJS / TEN) and acute generalized exanthematous pustulosis (AGEP)
Who gets drug hypersensitivity syndrome?
Drug hypersensitivity syndrome is relatively rare. It mainly affects adults and is the same in incidence in males and females. Genetic susceptibility and HLA associations have been found for several causal drugs.
The most common drugs to cause this reaction are a number of antiepileptic drugs (particularly carbamazepine, phenobarbital, and phenytoin), the anti-gout drug, allopurinol, olanzapine, and the sulfonamide group of antibiotics. It has been estimated that at least 1 in 10,000 patients treated with an anticonvulsant will develop drug hypersensitivity syndrome.
The risk of drug hypersensitivity syndrome in patients with allopurinol depends on the dose of allopurinol. It is higher if the patient has kidney disease and is also taking thiazide diuretics.
It has also been rarely reported to be due to other medications. It can be very difficult to determine the exact cause of drug hypersensitivity syndrome if multiple medications have been started in the past weeks. In approximately 10% of cases, the causal drug never identifies
What causes drug hypersensitivity syndrome?
Drug hypersensitivity syndrome is a delay T cell-mediated reaction. Tissue damage is due to cytotoxic T cells and cytokine launching.
- There's a genetic predisposition to drug hypersensitivity syndrome.
- A defect in the way the liver metabolizes drugs may be responsible.
- Reactivation of human herpes virus 6 (HHV6, the cause of roseola) or Epstein Barr virus (EBV) may also be important.
What are the clinical features of drug hypersensitivity syndrome?
Drug hypersensitivity syndrome usually develops over several days, with onset between 2 and 8 weeks after starting the responsible drug.
Usually a high fever of 38–40 C is first noted. This is quickly followed by a extended skin eruption. The characteristics of the eruption are diverse.
-
Morbilliform eruption affects 80% of cases, with different morphology even targettoid lesions, blisters and pustules
- Erythroderma or exfoliative dermatitis (involving> 90% of body surface area) can follow at about 10%
- Facial swelling affects 30%.
- Mucous membrane involvement affects 25% (lips, mouth, throat, genitals)
The rash can last for many weeks.
Rash drug hypersensitivity syndrome

Drug eruption

Drug eruption
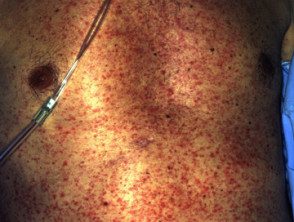
Drug eruption
Systemic compromise in drug hypersensitivity syndrome
Symptoms may get worse after stopping the drug and can continue for weeks or even months despite drug withdrawal. The severity of the rash does not necessarily correlate with the degree of involvement of the internal organs. Later symptoms depend on the internal organs affected. They may include:
- Enlarged lymph nodes multi-site (75%)
- Hematological disorders: elevated white count (or less commonly, reduced white count), eosinophilia (in 30% this is> 2.0 x 109 / L), atypical lymphocytes, thrombocytopenia, anemia, hemophagocytic syndrome
- Enlargement of the liver, hepatitis and rarely hepatic necrosis with liver failure Abnormal liver function tests are found in 70 to 90%
- Kidney disease: affects approximately 10% and is usually mild (interstitial nephritis) Renal failure is rare
- Inflammation of the heart (myocarditis) or cardiac sac (pericarditis), which causes chest pain, dyspnea, and low blood pressure
- Lung disease, causing shortness of breath and coughing (interstitial pneumonitis, pleurisy, pneumonia and acute respiratory distress syndrome)
- Neurological participation, which can lead to meningitis Y, encephalitis, polyneuritis, which causes headache, seizures, coma, and paralysis
- Gastrointestinal symptoms: stomach flu, pancreatitis, bleeding and dehydration. In severe, acute cases colitis and pancreatitis may occur, and chronic enteropathy may occur
- Endocrine abnormalities: thyroiditis and diabetes
- Muscle diseasemyositis)
- Eye disease (uveitis)
What are the complications of drug hypersensitivity syndrome?
Mortality from drug hypersensitivity syndrome is estimated to be around 8%. Causes of death include:
- Acute liver failure causes coagulation problems, jaundice and altered consciousness
- Multi-organic failure
- Fulminant myocarditis
- Hemophagocytosis
How is drug hypersensitivity syndrome diagnosed?
The diagnosis of drug hypersensitivity syndrome is based on the clinical presentation of the triad of:
- High fever
- Extensive skin rash
- Organ compromise
It is supported by eosinophilia and abnormal liver function tests.
As drug hypersensitivity syndrome can occur up to eight weeks after the first exposure to the responsible drug, a great deal of care is required in determining the responsible drug. A temporary The association between the use of medications and the onset of the syndrome is the strongest evidence.
The European Severe Skin Registry Adverse reactions Drug and Biological Sample Collection (RegiSCAR) has produced diagnostic criteria to aid in the diagnosis of drug hypersensitivity syndrome. RegiSCAR's inclusion criteria for potential cases require at least 3 of the following:
- Hospitalization
- Reaction suspected of being related to drugs
- Acute skin rash
- Fever above 38 C
- Enlarged lymph nodes at two sites
- Involvement of at least one internal organ
- Blood count abnormalities such as low plateletsraised eosinophils or abnormal lymphocyte tell
Attempts to confirm which drug has caused the drug hypersensitivity syndrome may include patch testing Patch testing has been reported to be most successful for antiepileptic drugs, with a 50% of positive reactions. Not useful for allopurinol, with 0% of positive reactions. The lymphocyte transformation test is available in some centers, where specialized interpretation can reveal the offending drug in most cases.
Research on drug hypersensitivity syndrome
After taking a careful history and performing a general and skin exam, the following tests may be ordered.
Skin biopsy usually shows dense infiltration of inflammatory cells, including lymphocytes and eosinophils, extravasated erythrocytesand edema.
Blood tests can include:
- Blood count and coagulation studies
- Biochemical tests: at least liver function, kidney function, muscle. enzymes
- Viral serology: hepatitis B, C, EBV, CMV, HHV-6
- Endocrine function: thyroid, glucose levels
A urinalysis is done to assess kidney damage.
Cardiac and pulmonary evaluation may include electrocardiograph (ECG), echocardiogramand chest x-ray. Scans may be done to evaluate the liver, kidneys, and brain based on symptoms and the results of initial tests.
What is the treatment for drug hypersensitivity syndrome?
Treatment consists of immediate withdrawal of all suspected medications, followed by careful monitoring and supportive care. It is very important that patients with high fever and rash, where it is considered a diagnosis of drug hypersensitivity syndrome, have blood tests as soon as possible.
Systemic steroids (eg, Prednisone) are generally used in the most severe cases of drug hypersensitivity syndrome involving significant exfoliative dermatitis, pneumonitis, and / or hepatitis. However, the benefits of corticosteroids are unknown as controlled clinical trials are lacking. Once effective, they must be withdrawn very slowly, as the syndrome may recur as the dose is reduced.
Cyclosporine has been reported to be an effective alternative treatment for drug hypersensitivity syndrome.
Additional treatment may include intravenous immunoglobulin, plasmapheresis and immunomodulator medications such as cyclophosphamide, mycophenolate, and rituximab.
Supportive treatment for the rash may include:
- Dressings
- Current corticosteroids
- Emollients
- Oral antihistamines.
Fluid, electrolyte, and calorie intake may need attention. A warm environment and skilled nursing care are required. Secondary infections may require antibiotics.
How can drug hypersensitivity syndrome be prevented?
Patients who develop drug hypersensitivity syndrome should avoid taking the offending drugs again.
Cross-reactions are common between the three main aromatic anticonvulsant medications (phenytoin, carbamazepine, and phenobarbitone), and patients who have experienced drug hypersensitivity syndrome with any of these medications should avoid all three.
Because genetic factors are suspected in drug hypersensitivity syndrome, first-degree relatives should be alerted to their high risk of developing hypersensitivity reactions to the same drugs.
What is the prognosis for drug hypersensitivity syndrome?
Most patients fully recover from drug hypersensitivity within weeks to months. Relapse After the initial improvement it is common.
Patients recovering from drug hypersensitivity syndrome are believed to be at risk of developing autoimmune diseases
