What is Hidradenitis suppurativa?
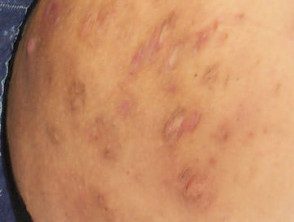
Hidradenitis suppurativa is a inflammatory skin disease that affects the skin with apocrine glands in the armpits, in the groin and under the breasts. It is characterized by recurrent how to boil nodules and abscesses that culminate in pus download, open wounds (breasts) difficult to heal and scars. Hidradenitis suppurativa also has a significant psychological impact, and many patients suffer from impaired body image, depression and anxiety.
The term hydradenitis implies that it begins as an inflammatory disorder of the sweat glands, which is now known to be incorrect. Hidradenitis suppurativa is also known as reverse acne.
Hidradenitis suppurativa

Hidradenitis suppurativa
Hidradenitis suppurativa

Hidradenitis suppurativa of armpit
See more images of Hidradenitis suppurativa.
Who gets Hidradenitis Suppurativa?
Hidradenitis often begins at puberty and is most active between the ages of 20 and 40, and in women, it can resolve at menopause. It is three times more common in women than in men. Risk factors include:
- Other family members with Hidradenitis suppurativa
- Obesity and insulin resistance / metabolic syndrome
- Smoking cigarettes
- Follicular occlusion disorders: acne conglobata, dissecting cellulitis, pilonidal breast
- Inflammatory bowel disease (Crohn's disease)
- Rare autoinflammatory syndromes associated with abnormalities of PSTPIP1 gene. *
* PAPA syndrome (pyogenic arthritis, pyoderma gangrenous and acne), PASH syndrome (gangrenous pyoderma, acne, suppurative hydradenitis) and PAPASH syndrome (pyogenic arthritis, gangrenous pyoderma, acne, hidradenitis suppurativa).
What causes Hidradenitis suppurativa?
Hidradenitis suppurativa is an autoinflammatory disorder. Although the exact cause is still not understood, contributing factors include:
- Clothes friction and body folds.
- Aberrant immune response to diner bacteria
- Abnormal cutaneous or follicular microbiome
- Follicular occlusion
- Break free from proinflammatory cytokines
- Inflammation causing rupture of the follicular wall and destroying apocrine glands and ducts
- Secondary bacterial infection
- Certain drugs.
What are the clinical characteristics of hidradenitis suppurativa?
Hidradenitis can affect single or multiple areas in the armpits, neck, submammary inner area and thighs. Anogenital the involvement most commonly affects the groin, pubis, vulva (in women), sides of the scrotum (in men), perineumbuttocks and perianal folds
The signs include:
- Open and close comedones
- Painful signature papules, larger nodules and pleated ridges
- Pustules, fluctuating pseudocysts and abscesses
- Pyogenic granulomas
- Breast drainage linking inflammatory lesions
- Hypertrophic and atrophic scars
Many patients with Hidradenitis Suppurativa also suffer from other skin disorders, such as acne, hirsutism, and psoriasis.
The severity and extent of hydradenitis suppurativa are recorded in evaluation and in determining the impact of treatment. The Hurley system describes three different clinical stages:
- Solitary or multiple, isolated abscess formation without scars or sinus tracts
- Recurrent abscesses, single or multiple widely separated lesions, with sinus tract formation
- Diffuse or broad participation, with multiple interconnected sinus tracts and abscesses.
Read more about assessing the severity of Hidradenitis Suppurativa.
Severe hydradenitis (Hurley Stage 3) has been associated with:
- Male sex
- Axillary and perianal involvement
- Obesity
- Of smoking
- Increased risk of stroke, coronary heart disease, heart failure, and peripheral arterial disease
- Duration of illness.
What is the treatment for Hidradenitis suppurativa?
General measures
- Weightloss; follow a anti-inflammatory, low sugar, low grain and low dairy diet (mainly plants)
-
Of smoking cessation: this can lead to improvement in a few months
- Baggy clothes
- Daily antiperspirants without perfume
- If you are prone to a secondary infection, wash with antiseptics or take bleach baths
- Apply hydrogen peroxide solution or medical grade honey to reduce bad odor
- Use peeling agents such as resorcinol at 15% cream to defrost nodules
- Apply simple bandages to the breasts to drain.
- Pain relievers, such as paracetamol (acetaminophen), for pain. control
- Seek help to control anxiety and depression.
Medical management of Hidradenitis suppurativa.
Medical treatment of Hidradenitis suppurativa is difficult. Long-term treatment is required. The effective options are listed below.
Antibiotics
- Current clindamycin, with benzoyl peroxide to reduce bacterial resistance
- A short course of oral antibiotics for acute staphylococcal abscesses (eg flucloxacillin)
- Long courses (three months minimum) of tetracycline, metronidazole, trimethoprim + sulfamethoxazole, fluoroquinolones, ertapenem or dapsone for their anti-inflammatory action
- 6-12 week courses of clindamycin (or doxycycline) and rifampin combination for severe disease.
Antiandrogens
- Long-term oral contraceptive pill; antiandrogenic progesterones Drospirenone or cyproterone acetate may be more effective than standard combination pills. These are more suitable than progesterone-only tablets or devices.
- Spironolactone and finasteride
- The answer takes six months or more.
Immunomodulator treatments for serious illnesses
-
Intralesional corticosteroids in nodules
- Systemic short-term corticosteroids for outbreaks
-
Methotrexate, cyclosporine, and azathioprine.
- Used in a higher dose than required for psoriasis, TNF-α inhibitor adalimumab is the most successful treatment to date. Note that, paradoxically, adalimumab can sometimes induce new-onset hidradenitis suppurativa.
- Other biologics are being investigated, such as the IL-1β antagonist, canakinumab.
Other medical treatments
- Metformin in patients with insulin resistance.
-
Acitretin (not suitable for women of childbearing age)
-
Isotretinoin: effective for acne, but seems useless for most cases of hydradenitis
- Colchicine
- Medical management of anxiety and depression.
Surgical management of Hidradenitis suppurativa.
- Incision and drainage of acute abscesses
-
Curettage and defrosting of nodules, abscesses and sinuses.
- To be ablation of nodules, abscesses and sinuses
- Wide local excision persistent nodules
- Radical excision surgery of the entire affected area
-
Nd: YAG laser hair elimination
