What is it hypogonadism?
Hypogonadism describes the improper function of the gonads (reproductive glands) leading to impaired germ cell production and sex hormones
What is hypogonadism in men?
Hypogonadism in men refers to decreased testicular function: a reduction in sperm production and in testosterone.
- Primary Hypogonadism is due to a disease that affects both testicles.
- Secondary hypogonadism is due to a disease of the hypothalamus or pituitary gland (hypogonadotropic hypogonadism).
What Causes Hypogonadism in Men?
Hypogonadism is due to disruption of any section of the hypothalamicPituitary pathway-gonadal axis (Figure 1).
- The hypothalamus produces gonadotropin-releasing hormone (GnRH).
- GnRH acts on the pituitary gland, which produces folliclestimulating hormone (FSH) and luteinizing hormone (LH).
- FSH stimulates spermatogenesis (sperm development) in the testes, and LH causes the production of testosterone.
Figure 1. The hypothalamic-pituitary-gonadal axis pathway
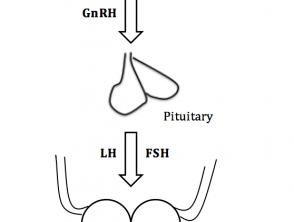
The hypothalamic-pituitary-gonadal axis pathway in men
FSH; follicle stimulating hormone, GnRH; Gonadotropin Releasing Hormone, LH; luteinizing hormone
Who gets hypogonadism?
Both primary and secondary hypogonadism in males can be congenital or acquired
Congenital primary hypogonadism
Signs of congenital primary hypogonadism include:
- Chromosomal abnormalities - the most common is Klinefelter syndrome (XXY karyotype)
- Cryptorchidism
- Myotonic dystrophy (muscle loss) - hypogonadism manifests itself in adulthood
- Varicocele (swelling of the veins in the scrotum)
- Disorders androgynous synthesis (rare)
Acquired primary hypogonadism
Acquired primary hypogonadism can be the result of:
- Infection, especially with mumps orchitis
- Medications, particularly for the use of alkylating agents, suramin, ketoconazole, and glucocorticoids
- Radiation
- Trauma
- Testicular torsion
- Autoimmune polyglandular syndrome type 1
- Chronic systemic liver disease cirrhosis, chronic kidney disease and human immunodeficiency virus (HIV) infection
- Idiopathic Causes
Secondary congenital hypogonadism
Congenital secondary hypogonadism results from isolated gonadotropin deficiency due to genetic mutationssuch as Kallmann syndrome, Prader-Willi syndrome, and other similar conditions.
Acquired secondary hypogonadism
Acquired secondary hypogonadism can result from:
- Damage to the pituitary or hypothalamus, including:
- Intracranial space-occupying lesions (eg, tumors and cysts)
- Infiltrative disease (eg, sarcoidosis and hemochromatosis)
- Infection (eg. meningitis)
- Pituitary apoplexy (bleeding in the pituitary gland)
- Trauma
- Gonadotropin suppression as a result of:
- Chronic illness (eg, Diabetes, anorexia, obesity and renal disease)
- Critical illness
- Chronic opiates glucocorticoidsor use of anabolic steroids
- Hyperprolactinemia (an excess of the hormone prolactin that induces milk).
What are the clinical features of hypogonadism in men?
The clinical features of hypogonadism depend on the age of the patient at presentation.
Testosterone deficiency at birth
Hypogonadism at birth can be recognized by ambiguous genitalia (external genitalia that are neither clearly male nor clearly female).
Testosterone deficiency before puberty
Hypogonadism prior to puberty can be diagnosed by the inability to undergo or complete puberty. The child may have a young appearance, pubis missing hair, he has small genitals and testicles, his voice may fail, and he may have trouble gaining muscle.
Testosterone deficiency after completing puberty.
After the completion of puberty, characteristics of hypogonadism include decreased libido, erectile dysfunction, osteoporosis, depression, gynecomastia, reduction of the testicles and infertility. After a few years of testosterone deficiency, decreased muscle mass and body hair may be evident.
What skin changes can be caused by hypogonadism in men?
Androgens are responsible for sebaceous gland growth and differentiation, hair growth and epidermal barrier homeostasis [1].
Androgen deficiency produces:
- Dry, thin and wrinkled skin.
- Lack of hair growth on the chest, armpit, face and genitals
- Lack of genitalia pigmentation
- Gynecomastia
- Reduced incidence of acne [2,3].
How is hypogonadism diagnosed in men?
The diagnosis of hypogonadism is based on the observation of the typical clinical characteristics in a man with low serum testosterone The patient should be referred to a specialist.
Initial investigations should include measurement of serum LH, FSH, and testosterone (usually taken in the morning and repeated at least twice). If testosterone is low:
- Elevated LH and FSH suggest primary hypogonadism
- Low levels of LH and FSH suggest secondary hypogonadism.
Further investigations should be directed to identifying the underlying cause.
What is the treatment and outcome of hypogonadism in men?
Effective testosterone replacement in hypogonadal men has been shown to maintain secondary sexual characteristics, increase libido, muscle strength, fat-free mass, and bone density [4].
The adverse effects of testosterone replacement include:
- Acne
- Enlarged prostate
- Stimulation of breast growth. Cancer or prostate cancer
- Sleep apnea
- Heart failure
- Erythrocytosis.
Which are the contraindications to testosterone therapy?
Testosterone should not be started in people with breast cancer, prostate cancer, or an increased risk of prostate cancer. hematocrit above 50%, untreated obstructive sleep apnea, severe lower urinary tract symptoms, or uncontrolled heart failure [4].
