What is the skin's immune system?
The skin has an immune system that protects the body from infection, Cancer, toxinsand try to prevent autoimmunity, in addition to being a physical barrier against the external environment.
The skin's immune system is sometimes referred to as skin-associated. lymphoid tissue (SAL), which includes peripheral lymphoid organs such as the spleen and lymph nodes.
Immune system of the skin
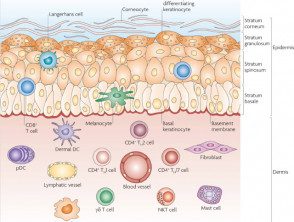
Anatomy of the skin and cell effectors.
Sentinel immune cells
Reprinted with permission from Macmillan Publishers.
How does the skin's immune system work?
The skin's immune system has elements of both the innate (non-specific) immune system and the adaptive (specific) immune system. Immune cells inhabit the epidermis and dermis.
The key immune cells in the epidermis are:
- Epidermal dendritic cells (Langerhans cells)
- Keratinocytes (skin cells).
The dermis has blood and lymphatic vessels and numerous immune cells, including:
- Dermal dendritic cells
- Lymphocytes: T cells, B cells, natural killer (NK) cells
- Mast cells.
There is a continuous traffic of immune cells between the skin, the drainage of the lymph nodes and the blood circulation. The skin microbiome also contributes to homeostasis of the skin's immune system.
What is the skin's innate immune response?
The innate immune response is immediate and is not dependent in previous immune memory.
Keratinocytes
Keratinocytes are the predominant cells in the epidermis. They act as the first line of innate immune defense against infection. Express Toll-like receptors (TLRs), which are pattern recognition receptors (PRRs) that detect conserved molecules in pathogens and trigger a inflammatory reply.
Keratinocytes communicate with the rest of the immune system through:
- Antimicrobial peptides (cathelicidins and β-defensins)
- Signaling cytokines (e.g, interleukin–1β [IL-1β])
- Chemokines, which attract other immune cells to the epidermis
- Direct activation of priming T lymphocytes and NK cells (via major histocompatibility complex I [MHC-I])
Macrophages and neutrophils
Macrophages are phagocytic cells that can discriminate between the body's cells (own) and foreign molecules. After phagocytosis by macrophages, an invasion pathogen he is assassinated inside the cell. Activated macrophages recruit neutrophils to enter the circulation and travel to sites of infection or inflammation.
Neutrophils are the first cells to respond to infection. They attack directly microorganisms by phagocytosis and by degranulation of toxic substances
Dendritic cells
Epidermal and dermal dendritic cells are involved in innate and adaptive immune responses. During the innate response:
- Dendritic cells possess TLRs that can be activated by microbial components.
- Plasmacytoid dendritic cells (pDC) produce large amounts of interferon-γ (IFN-γ) in response to viral infection.
Natural killer cells
NK cells are cytotoxic lymphocytes that can kill virus-infected cells and cancer cells without antigen presentation or priming.
NK cells are activated by interferons or other cytokines released by macrophages. NK cells express inhibitory receptors that recognize MHC-I and prevent undesirable attacks against the self. They can kill target cells via the perforin-granzyme pathway, which induces apoptosis (programmed cell death).
Mast cells
Mast cells are activated in response to allergic reactions and produce cytoplasm granules filled with preformed inflammatory mediators, as histamine. They release these granules when their high affinity immunoglobulin E (IgE) receiver (FcεRI) in the mast cells the surface reacts to contact with stimuli such as Allergens, poisons, IgE antibodiesand medications.
These mediators can result in pruritus cure due to increase vascular permeability (urticaria) In rare cases, mast cell activation can lead to anaphylaxis, Characterized by bronchoconstriction, dizziness and syncope.
Eosinophils
Eosinophils enter the skin in pathological conditions such as parasitic infestations and atopic dermatitis. Eosinophils are attracted to immunoglobulins as IgE you are required to complement proteins on the surface of large organisms how helminths.
Eosinophils release cytoplasmic cytotoxic granules to kill the parasite (an innate immune response) and promote Th2 helper T cell differentiation upon release (an adaptive immune response).
Complementary system
The complement system is a enzymatic cascade of more than 20 different proteins normally found in the blood. When an infection is present, the system is activated sequentially and leads to events that help destroy the invasion. organism.
The complement system can also attract neutrophils to the site of infection.
What is the adaptive immune response?
The adaptive immune response is specific to a pathogen and takes longer to elicit. Adaptive immunity requires the production of specific T lymphocytes to accurately identify an antigen and B cells to produce specific antibodies that bind to it. microbe in a 'lock and key' form.
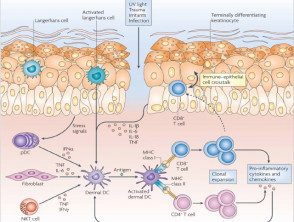
Antigen presentation
Dendritic cells (Langerhans cells and macrophages), or antigen presenting cells (APCs), identify antigens and present them to immature T cells. Epidermal Langerhans cells use their dendrites (arm-shaped projections) to examine the environment, especially in the stratum corneum. Langerhans cells bind pathogens to their TLRs, travel to draining lymph nodes, and present antigens to naive lymphocytes. Antigen presentation requires internalization of the pathogen, processing within the cell, and visualization of a brief peptide on the surface of the APC in an important histocompatibility complex (MHC) molecule.
There are two main types of MHC: MHC-I and MHC-II.
- MHC-I is found in all cells of the body and is used to show endogenous substances, such as viruses or tumor protein
- MHC-II is found in APC (dendritic cells, monocytes/ macrophages and B cells) and is used to display non-self foreign molecules.
T cells
The skin contains resident T cells and recruits circulating T cells. T cells cannot recognize pathogens directly. The receptor on the surface of a T cell binds to the peptide / MHC complex on the surface of the APC. Efficient antigen presentation allows naive T cells to mature into effector T cells, which in turn differentiate into two varieties: cytotoxic CD8 + T cells and helper (Th) CD4 + T cells.
Cytotoxic CD8 + T cells recognize and bind to MHC-I molecules. They bind to the death receptor Fas, a protein on the surface of the cell membrane that initiates the perforin-granzyme pathway and cytokine-mediated pathways to induce apoptosis, which directly kills virus-infected cells or tumor cells.
CD4 + Th cells recognize and bind to MHC-II molecules. They activate B cells to produce specific antibodies. Upon re-exposure to the same antigen, memory T cells can respond rapidly by dividing and clone expansion.
Th cells include the Th1, Th2, Th17, and Th22 subtypes. Each subtype is associated with specific signaling cytokines and effector functions.
Th1 cells produce a cell-mediated immune response to kill intracellular pathogens
- Th1 cells produce IFN-γ and can activate macrophages and stimulate NK cells.
- Th1 cells play a role in Pathogenesis psoriasis
Th2 cell activation leads to Cell B stimulation and antibody production.
- Th2 cells produce cytokines IL-4, IL-5, IL-6, and IL-10.
- They can stimulate eosinophils activation.
- Th2 cells are involved in the atopic. eczema.
Th17 cells produce IL-17 and IL-22 and play a role in protection against bacterial infections and fungal infections. Th22 cells produce IL-22 and tumor necrosis alpha factor (TNF-α), which induces inflammation. Th17 and Th22 cells play a role in the pathogenesis of psoriasis. Other populations of T cells, such as regulatory T cells (Tregs), adjust the immune response by controlling the response of immune cells to foreign cells and autoantigens and prevent autoimmune reactions.
B cells
B cells are responsible for creating a memory of previous antigen exposure to ensure a faster immune response and long-lasting immunity. B cells produce antibodies (immunoglobulins) that can bind to specific antigens. The effector functions of antibodies are:
- Neutralization - Antibodies bind to the pathogen and prevent adherence / infection
- Opsonization: the coating of the antigen surface by antibodies and subsequent uptake by phagocytic cells
-
Activation plugin.
To produce antibodies, B cells require cytokine signaling and Th cell stimulatory signals. This takes place in secondary lymphoid organs such as lymph nodes.
- B cells and T cells must bind through the B cell receptor (BCR) and the T cell receptor, respectively. This is mediated by costimulatory signals in Th cells.
- the proliferation of B cells leads to the production of a specific antibody, either IgG, IgA or IgE, depending on the antigen.
After re-exposure to the same antigen and follicular dendritic cells, B cells are activated to produce specific antibodies. This process allows the generation of memory and long-lasting B cells. plasma cells for long-lasting immunity against infection.
