What are they cutaneous T cell lymphomas?
Lymphomas are tumors of the lymph nodes and lymphatic system. Extranodal Lymphomas are tumors that occur in organs or tissues outside the lymphatic system. When lymphomas occur on the skin without evidence of disease anywhere else at the time of diagnosis, they are called 'primaryCutaneous lymphomas. There are many different types of primary cutaneous lymphomas, but they can be broadly divided into two categories, cutaneous T-cell lymphomas and cutaneous B-cell lymphomas. Of all the primary cutaneous lymphomas, 65% are of the T-cell type.
Cutaneous T-cell lymphomas (CTCL) refer to a rare but serious skin condition in which there is an abnormality. neoplastic proliferation of lymphocytes with a subtype 'T' (derived from the thymus). The diagnosis is made by the skin. biopsy.
Classification of cutaneous T-cell lymphomas
Recently, the World Health Organization (WHO) and the European Organization for Research and Treatment of Cancer The classification (EORTC) reached a consensus classification for cutaneous lymphomas [1] and reviewed by the WHO in 2008 [2]. Cutaneous T-cell lymphomas are divided into the following classifications.
| Indolent (low grade / slow growth) clinical behavior | Aggressive clinical behavior. |
|---|---|
|
|
Mycosis fungoides is the most common type of CTCL and represents almost 50% of all primary cutaneous lymphomas. The second most common group of CTCLs are primary cutaneous CD30 + lymphoproliferative disorders.
Mycosis fungoides
Mycosis fungoides is a condition in which the skin is infiltrated by patches or lumps made up of white blood cells called lymphocytes. It is more common in men than women and is very rare in children. Its cause is unknown, but in some patients it is associated with a pre-existing contact allergy. dermatitis or infection with a retrovirus
Mycosis fungoides has an indolent (low-grade) clinical course, which means that it can persist at one stage or for years, or sometimes decades, slowly progress to another stage (from patches to thicker ones). plates and eventually tumors).
The name of mycosis fungoides is historical and confusing: cutaneous T-cell lymphoma has nothing to do with yeast infection.
Patch stage
At the stage of mycosis fungoides patch, the skin lesions are flat. Most of the time they are oval or ring-shaped (cancel) dry pink patches on the covered skin. They may spontaneously disappear, remain the same size, or slowly enlarge. The skin can be atrophic (thinned), and may or may not itch. The patch stage of mycosis fungoides can be difficult to distinguish from psoriasis, discoid eczema or parapsoriasis
Mycosis fungoides stage patch

Mycosis fungoides

Mycosis fungoides

Mycosis fungoides
See more images of cutaneous T-cell lymphoma.
Poikiloderma vascular atrophy
Poikiloderma atrophicans vasculare is an unusual variant in which the skin shows areas of thinning, pigment change, and skin dilation. capillaries (telangiectasia)
Poikiloderma vasculare atroficans

Mycosis fungoides

Mycosis fungoides

Mycosis fungoides
License plate stage
In the mycosis fungoides plaque stage, the patches thicken and may resemble psoriasis. They tend to itch.
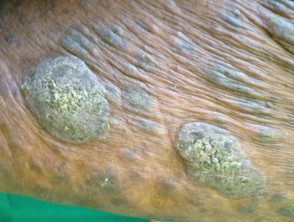
Mycosis fungoides plaque stage

Mycosis fungoides

Mycosis fungoides

Mycosis fungoides
See more images of Cutaneous T-Cell Lymphoma.
Tumor stage
In the tumor stage, mycosis fungoides, large irregular lumps develop from plaques de novo. They can ulcerate. At this stage, spread to other organs is more likely than in earlier stages. The type of tumor can develop into large cell lymphoma.
Mycosis fungoides tumor stage

Mycosis fungoides

Mycosis fungoides
mycosis fungoides 18
See more images of Cutaneous T-Cell Lymphoma.
MF variants and subtypes
There are a number of variants and subtypes of mycosis fungoides. Most follow the same clinical and pathological features as MF, but some have distinctive features as described below.
| Variant / subtype | Clinical / pathological characteristics. |
|---|---|
| Folliculotropic MF (follicular cell lymphoma) |
|
| Pagetoid reticulosis |
|
| Granulomatous loose skin |
|
| Mycosis fungoides palmaris and plantaris |
|
Primary cutaneous CD30 + lymphoproliferative disorders
This is the second most common CTCL group and represents approximately 30% of all CTCL cases. This group includes primary cutaneous anaplastic large cell lymphoma and lymphomatoid papulosis.
| Primary anaplastic cutaneous large cell lymphoma | Lymphomatoid papulosis |
|---|---|
|
|
CD30 + lymphoproliferative disorders

Anaplastic large cell lymphoma
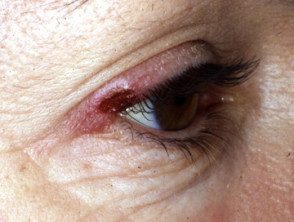
Lymphomatoid papulosis

Lymphomatoid papulosis
Sézary syndrome
Sézary syndrome is the name given when T-cell lymphoma affects the skin of the entire body. It is also known as red man syndrome because the skin is bright red. The skin is also thickened, dry or scaly and usually itches a lot. Examination generally reveals the presence of neoplastic T cells (Sézary cells) in the skin, enlarged lymph nodes, and peripheral blood. The prognosis for Sézary syndrome is generally poor with a median survival of 2 to 4 years. Most patients die of opportunistic infections that are due to immunosuppression.
Sézary syndrome
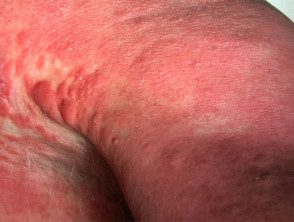
Sezary syndrome

Sezary syndrome

Sezary syndrome
Adult T-cell leukemia / lymphoma
Adult T-cell leukemia / lymphoma (ATLL) is a serious blood disease in which there are a large number of circulating cells. atypical cells. It is caused by a retrovirus infection with the human T lymphotropic virus (HTLV I). The condition can be divided into acute and chronic types. Acute ATLL is characterized by skin lesions similar to those found in mycosis fungoides or Sézary syndrome, enlarged lymph nodes, high levels of calcium in the blood, and bone lesions. The prognosis is poor for this type with a survival that varies from 2 weeks to more than 1 year. Chronic ATLL presents only with skin lesions and has a longer clinical course and survival, however, this can transform into an acute phase with an aggressive course.
What research should be done on cutaneous T-cell lymphoma?
Diagnosis of cutaneous T-cell lymphoma is made clinically and confirmed by a dermatopathologist (see mycosis fungoides pathology) There are characteristics microscopic changes observed in skin biopsy. Diagnosis is often delayed for months or years and may require several biopsiesBecause early cutaneous T-cell lymphoma can be difficult to distinguish from other skin conditions, particularly eczema.
Enlarged lymph nodes can also be biopsied. Cutaneous T-cell lymphoma can cause harmless swelling, known as 'reactive' or 'endopathic' lymphadenopathyor result evil one growth in lymph nodes.
The blood count is normal in most patients with cutaneous T-cell lymphoma, but an elevated white blood cell count is characteristic of Sézary syndrome. Some patients may undergo bone marrow. Aspire or biopsy
Patients with advanced cutaneous T-cell lymphoma may have Connecticut or Magnetic resonance Scans to determine if the disease affects the internal organs.
What is the treatment for cutaneous T-cell lymphoma?
Treatment of individual patients varies and depends on the stage, local experience, and available medications and equipment. The following may be useful.
- Current steroids
- UVB phototherapy
- PUVA photochemotherapy
- Topical Nitrogen Mustard
-
Bexarotene gel (a topical rexinoid)
- Chemotherapy
- Located radiotherapy
- Electron beam radiation therapy
- Interferons
- Oral retinoids
- Gemcitabine, a pyrimidine analog term, which can be combined with other chemotherapy agents
-
Extracorporeal photopheresis.
- Allogenic stem cells transplant
What is the prognosis for T-cell lymphoma?
Cutaneous T-cell lymphoma can remain confined to the skin for many years, but abnormal cells can eventually infiltrate other tissues, such as blood, lymph nodes, lungs, heart, liver, and spleen.
Unlike other lymphomas, the prognosis is generally good. Symptoms can generally be controlled with treatment. However, the treatment is not curative.
