What is lupus erythematosus?
Lupus erythematosus (LE) is a connective tissue disease and autoimmune disorder that can affect one or more organs. Circulating autoantibodies and immune complexes are due to loss of normal immune tolerance and are pathogen. The clinical characteristics of LE are highly variable. LE almost always affects the skin to some degree.
What is it cutaneous lupus erythematosus?
Cutaneous LE comprises several chronic and LE-specific and non-LE-specific relapse inflammatory conditions There may be some overlap.
-
LE-specific cutaneous LE has been classified as acute, subacute, intermittent and chronic. Injuries can be located or generalized. In LE-specific cutaneous LE, lesions are often induced by exposure to sunlight.
-
Nonspecific cutaneous LE-LE may be related to systemic LE or other autoimmune disease.
Who gets cutaneous lupus erythematosus?
Cutaneous LE most often affects young and middle-aged adult women (ages 20-50), but children, the elderly, and men can be affected.
Important predisposing factors for cutaneous LE include:
- Female sex
- Genes: ≥ 25 risk loci have been identified, and there are HLA associations
- Colored skin.
What Causes Lupus Erythematosus?
LE is classified as an autoimmune disorder, as it is associated with pathogens antibodies directed against cell components nuclei on various tissues Causes of UVB irradiation keratinocytes necrosis, activation of the immune system and antibody training.
Factors that aggravate LE include:
- Sun exposure
- Smoking cigarettes
- Hormones
- Viral infection
- Certain drugs.
What are the specific characteristics of cutaneous lupus erythematosus?
There are several types of cutaneous LE, classified as acute, subacute, intermittent, and chronic cutaneous LE. The revised Cutaneous Lupus Erythematosus Severity Index and Area Index (RCLASI) can be used to assess disease activity and damage.
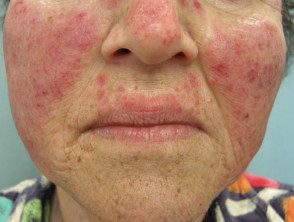
Acute cutaneous lupus erythematosus
Acute cutaneous LE affects at least 50% in patients with systemic lupus erythematosus (SLE). Many are sick, young, fair-skinned females.
Specific features of acute cutaneous LE may include:
- Malar eruption o 'butterfly eruption'(erythema and edema of cheeks, preserving nasolabial folds) that last hours to days
- Erythematous papular rash on the arms, sometimes forming large plates and spreading widely
- Photosensitivity (An eruption around the sun recentlyexposed skin)
-
Cheilitis and mouth ulcers
- Blisters (bullous SLE) and erosions.
SLE can also affect joints, kidneys, lungs, heart, liver, brain, blood vessels (vasculitis) and blood cells. May be accompanied by antiphospholipid syndrome.
Systemic LE

Systemic LE

Systemic LE

Systemic LE
See more pictures of systemic lupus erythematosus.
Subacute cutaneous lupus erythematosus
About 15% of patients with cutaneous LE have subacute cutaneous LE. One third of the cases are due to previous exposure to drugs.
Features of subacute cutaneous LE include:
- Precipitation or aggravation from sun exposure
- Not itchy like psoriasis papulosquamous rash on the upper back, chest, and upper arms
- Cancel or polycyclic plates clearing centrally
- The absence of scars when the rash has resolved.
Up to 50% of patients with subacute cutaneous LE may also have a mild form of SLE, resulting in arthralgia (painful joints) or arthritis (joint disease) and low blood counts. Severe SLE is rare in patients with subacute cutaneous LE.
Subacute LE
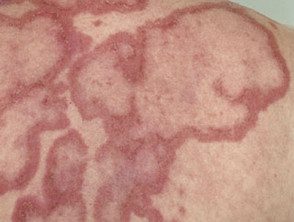
Subacute cutaneous LE
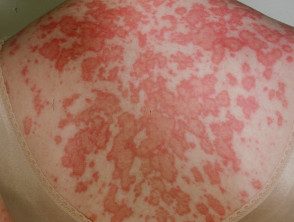
Subacute cutaneous LE

Subacute cutaneous LE
Drug-induced subacute cutaneous LE
More than 100 drugs have been associated with the development of drug-induced lupus, and the majority present with subacute cutaneous LE. They include:
- Terbinafine
- Tumor necrosis factor alpha (TNF-α) inhibitors (biologics)
- Anticonvulsants
- Proton-pump inhibitor.
Drug-induced lupus
Drug-induced lupus

Drug-induced lupus
Drug-induced lupus
Neonatal cutaneous lupus erythematosus
Neonatal cutaneous LE arises within 2 months of birth to mothers with subacute, subacute, or subclinical cutaneous LE.
Features of neonatal cutaneous LE may include:
- Erythematous annular rash, which resolves slowly over 6 months.
- The rash is more frequent. periorbital
- Photosensitivity
- Blood count abnormalities: hemolytic anemia, leukopenia, thrombocytopenia
- Hepatobiliary disease
- Persistent congenital heart block
A pediatrician should evaluate all babies born to mothers with subacute LE (or carriers of anti-Ro / La) at birth. Mortality in infants with heart block is up to 20%, despite pacemaker implantation.
Neonatal lupus

Neonatal lupus

Neonatal lupus

Neonatal lupus
Intermittent cutaneous lupus erythematosus
Intermittent cutaneous LE, more often known as lupus tumidus, is a dermal form of lupus
Characteristics of lupus tumidus include:
- It affects places exposed to the sun such as cheeks, neck, previous chest
- Erythematous urticaria-like patches and plates with a smooth surface
- Round or ring shapes
- It clears during the winter months.
- No scars.
Lupus tumidus is similar to Jessner lymphocytic infiltrate, in which the diagnostic criteria for lupus are absent.
Lupus tumidus

Lupus tumidus
Chronic cutaneous lupus erythematosus
Chronic cutaneous LE represents the 80% of cutaneous LE presentations. About 25% of patients with chronic cutaneous LE also have systemic LE.
Discoid YOU
Discoid LE is the most common form of chronic cutaneous LE. It's more predominant in patients with colored skin, at increased risk of post-inflammatory hyperpigmentation and hypertrophic scars
- Discoid LE is confined to the skin over the neck in most patients, but can spread below the neck to affect the upper back, V-neck, forearms, and back of the hands.
- The scalp, ears, cheeks, and nose are the most common sites.
- Most patients have photosensitivity.
- The new lesions are destructive, erythematous. scaly plates with follicular prominence.
- Discoid LE scalp presents as red, scaly, and bald patches.
- Slow healing leads to post-inflammatory pigmentation and white scars.
- Hair growth can be partially or completely recovered with treatment. Cicatricial (scars) alopecia can be permanent
Hypertrophic LE
Hypertrophic LE is a variant of discoid LE in which there is thickening and warty plaques resembling viral warts or skin cancers. Hypertrophic LE can occur on the palms and / or soles of the feet. This is also called palmoplantar LE and is a form of acquisition keratoderma.
Mucous membrane YOU
The LE mucosa presents with plaques, ulcers and climbing. Mucosal lesions can predispose to scaly cell carcinoma. Common sites are:
- Lips and inside the mouth.
- Lower eyelid with madarosis (loss of eyelashes)
- Rarely, vulva/penis.
Discoid lupus erythematosus

Discoid LE

Discoid lupus erythematosus

Discoid lupus erythematosus
See more images of cutaneous lupus erythematosus.
Deep lupus
Deep lupus affects subcutaneous tissue. Other names for deep lupus are lupus panniculitis and subcutaneous LE.
- Deep lupus can develop at any age, even childhood.
- It can involve the face, buttocks, extremities, or anywhere.
- Firm deep and tender nodules persist for a few months.
- Injuries are resolved leaving dented, atrophic scars (lipoatrophy).
Deep lupus

Lupus panniculitis

Lupus panniculitis

Lupus panniculitis
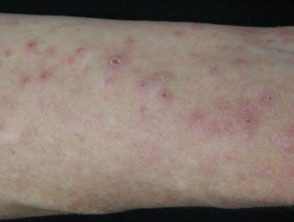
What are the nonspecific skin characteristics of lupus erythematosus?
Nonspecific skin characteristics of LE are more frequently associated with SLE. They include:
- Diffuse hair thinning
- Urticaria
- Raynaud's phenomenon: abnormal pallor of fingers and toes in response to cold weather, followed by numbness and slow rewarming of the fingers turning blue and then red.
-
Chilblains lupus erythematosus: painful erythematous nodules on the fingers and toes during colder months.
- Expanded periungual telangiectasia, uneven cuticles and nails dystrophy
- Digital ulcers and bites scars
- Thrombophlebitis
- Papular and nodular mucinosis on the cheeks, upper chest, upper arms, or back.
-
Vasculitis: small vessel vasculitis, urticarial vasculitis and less commonly, medium and large vessel vasculitis
- Livedo reticularis and antiphospholipid syndrome.
Chilblains lupus

Chilblains lupus

Chilblains lupus

Chilblains lupus
What are the complications of cutaneous lupus erythematosus?
Chronic skin LE causes facial deformity and scarring. Active and exhausted illness can lead to social isolation and depression.
Systemic LE can involve the heart, lung, and brain with morbidity and mortality. Vasculitis and antiphospholipid syndrome affecting internal organs can be serious.
How is cutaneous lupus erythematosus diagnosed?
-
SLE is associated with high-titer antinuclear antibodies.
- About 70% of subacute LE patients have removable anti-Ro / La nuclear antigens (ENA)
- The severity of LE can be reflected in the ANA and / or ENA title.
- ANA and ENA are often negative in a patient with chronic cutaneous LE.
- Mild anemia or leukopenia may be present in patients who do not have SLE
A skin biopsy may be diagnostic, showing a lichenoid tissue reaction and specific characteristics of the skin LE type. Direct immunofluorescence tests may show positive antibodies statement along the basement membrane (lupus band test).
Diagnostic features on biopsy are more likely to be found in LE-specific skin lesions than in LE non-specific cutaneous LE.
Note: All women with positive anti-Ro or anti-La antibodies should be warned that if they become pregnant there may be a risk to their baby of developing neonatal lupus and congenital heart block. Women with these antibodies should be referred to an obstetrician and should be considered prophylactic administration of
> hydroxychloroquine or low dose prednisone to prevent heart block in the fetus.
How can cutaneous lupus erythematosus be prevented?
- Carefully protect all exposed skin from sun exposure with protective clothing and broad spectrum sunscreen SPF50 + (see sun protection).
-
Of smoking cessation is essential: it is best to avoid nicotine replacement as nicotine in any form can exacerbate Cutaneous LE.
- If subacute LE is drug-induced, discontinue responsible medication.
What is the treatment for cutaneous lupus erythematosus?
The goal of treatment for cutaneous LE is to prevent breakouts, improve appearance, and prevent scars.
Local therapy
- Powerful or ultra-powerful current steroids are applied to discoid chronic LE plaques.
-
Calcineurin inhibitors, pimecrolimus cream or tacrolimus ointment can be used in place of topical steroids.
-
Intralesional corticosteroid can be injected into small lesions resistant to topical therapy.
-
Current retinoidsCalcipotriol and imiquimod have also been reported to be helpful in some patients.
-
Cosmetic camouflage can be used to disguise unsightly plates.
Systemic therapy
Treatment for cutaneous and systemic LE may include:
-
Antimalarials especially hydroxychloroquine
- Immune modulators such as methotrexate, mycophenolate, dapsone, cyclosporine
-
Retinoids, that is, acitretin, isotretinoin.
- Systemic corticosteroids
- If sun protection is strict, supplementation with vitamin D.
Severe illness may require more aggressive treatment:
- Cyclophosphamide
- Thalidomide
- Photopheresis
- Intravenous immunoglobulin
- Monoclonal antibodies directed at T and B cells and cytokines: rituximab.
Procedures
-
UVA1 phototherapy may be useful for treating LE cutaneous lesions.
- Photodynamic The therapy (PDT) has been reported to eliminate chronic cutaneous LE.
- A vascular To be can reduce telangiectasia
- Surgery can improve the appearance of disfiguring scars.
What is the prognosis for cutaneous lupus erythematosus?
the forecast for cutaneous LE it is variable.
Skin involvement in SLE tends to reflect systemic involvement.
Drug-induced SCLE disappears within a few weeks of withdrawal of the responsible drug.
Untreated chronic cutaneous LE tends to persist, but the severity is reduced by strict sun protection and avoidance of nicotine.
