What is vaginitis?
The term 'vaginitis' means an inflamed vagina; the term is freely used to refer to any vaginal condition that causes download, either for infectious or non-infectious causes.
What is it aerobic vaginitis?
Aerobic vaginitis is characterized by:
- Vaginal inflammation
- Atrophy vaginal epithelium
- Abnormal vaginal microflora including:
- Increased aerobic levels. bacteria
- Decreased levels of lactobacilli.
Aerobic vaginitis was first characterized by Donders et al in 2002. flaking inflammatory Vaginitis is a serious form of aerobic vaginitis. [1,2].
Who gets aerobic vaginitis?
Aerobic vaginitis can affect adult women of any age, either before or after menopause. the predominance of aerobic vaginitis has been estimated in different populations as present in 5 to 13% of asymptomatic women and affecting a higher proportion of women with vaginal symptoms. It can be less predominant among pregnant women.
Risk factors for infection are under evaluation
What is the cause of aerobic vaginitis?
The cause of aerobic vaginitis is unknown. Aerobic vaginitis is a form of dysbiosis, a disturbance in the ecology of micro-aerobiaorganisms residing in the vaginal microflora (the microbiome) These microorganisms include:
- Escherichia coli
- Staphylococcus aureus
- Coagulasenegative staphylococci (eg, S. epidermidis)
- Streptococcus agalactiae
- Enterococcus faecalis.
It is not clear whether the primary the cause of aerobic vaginitis is pathogen organisms, lack of lactobacilli, immune deregulation and proinflammatory cytokinesor insufficient estrogen in the vagina mucous membrane (atrophic vulvovaginitis) [2].
What are the clinical features of aerobic vaginitis?
Aerobic vaginitis symptoms can fluctuate over a long period of time. They include [2]:
- Vaginal stings and burning sensations
- Dyspareunia
- A sticky yellow or green discharge with a rotten smell.
Exam results may include:
- Vaginal inflammation (introital and vaginal redness, edema, and sometimes, petechiae and ecchymosis)
- Vaginal epithelial breaking off (erosions and ulcers)
- Vaginal augmentation pH.
What are the complications of aerobic vaginitis?
Aerobic vaginitis has been associated with [2]:
- Other forms of vaginitis
- Infection-related miscarriage, premature rupture of membranes, ascending chorioamniotis (inflammation around the fetus), and premature delivery
- Activation of human and cervical papillomavirus infection Cancer, possibly due to the increase in pH and the lack of lactobacilli
- Increased risk of contracting sexually transmitted infections, due to erosions in the vaginal mucosa.
- Pelvic inflammatory disease and infertility. [4].
How is aerobic vaginitis diagnosed?
The diagnosis of aerobic vaginitis is confirmed by wet mounting microscopy of fresh vaginal fluid, ideally using phase contrast. The aerobic vaginitis score is classified as 0–3 (absent), 3–4 (mild), 5–6 (moderate), and 6–10 (severe). The aerobic vaginitis score is calculated from [1]:
- Lactobacillary grade (LBG): I - III, namely (I) numerous pleomorphic lactobacilli, without other bacteria; (IIa) mixed flora, but predominantly lactobacilli; (IIb) mixed flora, but the proportion of lactobacilli decreased severely due to the increase in the number of other bacteria; and (III) severely depressed or absent lactobacilli due to the overgrowth of other bacteria
- Number of leukocytes compared to epithelial cells
- Proportion of toxic leukocytes (these are recognized by their cytoplasm granules)
- Characteristics of the microflora (eg, coconuts and coliforms)
- Presence of immature or parabasal epithelial cells (the cells most commonly seen on a vaginal smear).
Vaginal cultures are useful only for clinical research and for detecting group A streptococci, trichomoniasis, and Candida albicans infection.
Several advanced diagnostic methods for aerobic vaginitis are being established.
Phase contrast microscopy of aerobic vaginitis
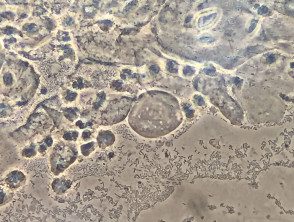
Aerobic vaginitis
* Credit: Pedro Vieira Baptista
Which is the differential diagnosis for aerobic vaginitis?
Aerobic vaginitis is different from other forms of infectious vaginitis, particularly bacterial vaginosis, with which it is often confused. The characteristics of bacterial vaginosis are:
- Lack of symptoms
- Grayish-white, watery discharge with a fishy odor.
- Lack of inflammation on vaginal examination.
- Microscopic findings of decreased lactobacilli and granular flora.
What is the treatment for aerobic vaginitis?
The treatment of aerobic vaginitis depends on microscopic findings and needs of the patient [2].
- Current corticosteroids (eg, hydrocortisone cream or foam) are used to treat a prominent inflammatory component (i.e.> 20 leukocytes per epithelial cell under microscopy).
- Antimicrobial (topical, oral or suppository) are used to eradicate pathogenic bacteria; These may include:
- An antiseptic (eg, dequalinium chloride)
- Topical antibiotic (eg, topical kanamycin or clindamycin; note that clindamycin may promote bacterial resistance)
- An oral antibiotic (eg, Amoxicillin-clavulanic acid or moxifloxacin).
- Topical estrogen is used to treat vaginal atrophy (that is, when parabasal cells are> 10% from epithelial cells under microscopy).
- Vaginal probiotics are used to restore vaginal lactobacilli.
Metronidazole, which is used for bacterial vaginosis, and antifungal agents, used to Candida albicans infection, they are not effective in aerobic vaginitis.
The advice of a medical microbiologist should be sought in pregnant women with aerobic vaginitis.
