What is it cutaneous Cell B lymphoma?
Lymphomas are tumors of the lymph nodes and lymphatic system.
- Extranodal Lymphomas are tumors that occur in organs or tissues outside the lymphatic system.
- Primary cutaneous lymphomas occur on the skin without evidence of extracutaneous disease at diagnosis.
Primary cutaneous lymphoma can be divided into two categories:
- Cutaneous T cell lymphoma
- B cell lymphoma.
Primary cutaneous B-cell lymphomas (PCBL) comprise approximately 20% of cutaneous lymphomas and are described on this page.
What are cutaneous B-cell lymphomas?
Cutaneous B-cell lymphomas are a evil one proliferation of lymphocytes B cell type. Mutation what happens at different points of Cell B Development leads to different forms of lymphoma.
In 2005, the World Health Organization (WHO) and the European Organization for Research and Treatment of Cancer The classification (EORTC) reached a consensus classification for cutaneous lymphomas. It was reviewed by the WHO in 2008. The three main types of PCBCL are:
- Primary dermal follicle central lymphoma (PCFCL)
-
Primary dermal marginal zone B- cell lymphoma (PCMZL)
- Primary dermal diffuse Large B-cell lymphoma, leg type (PCDLBCL-LT).
Rare cases of PCDLBCL that do not belong to the PCDLBCL-LT or PCFCL groups are classified as PCDLBCL-other. Other entities like anaplastic or plasmablastic lymphoma, primary cutaneous T cells Rev.histiocyterich in B-cell lymphomas and primary cutaneous intravascular Large B-cell lymphomas are very rare.
Due to differences in treatment and forecast, it is important to discern between PCBCL and systemic forms of B-cell lymphomas that manifest with secondary skin involvement.
Cutaneous B-cell lymphoma

Lymphoma FC

Cutaneous B-cell lymphoma

Cutaneous B-cell lymphoma
Who gets cutaneous B-cell lymphoma?
Primary cutaneous lymphoma of the follicular center
- Primary Lymphoma of the Cutaneous Follicular Center (PCFCL) It is the second most common lymphoma in the western world.
- It is the most common type of PCBCL.
- It has a 5-year survival of approximately 95%.
- It affects older patients, median age 60 years.
Primary cutaneous B-cell lymphoma of the marginal zone
See B-cell lymphoma of the primary cutaneous marginal zone (PCMZL).
- Men are affected twice as much as women.
- Some are associated with Borrelia burgdorferi infection (the cause of Lyme disease) in endemic areas of Europe and the United States.
- It has the best 5-year survival of the 99%.
- Younger patients are affected, with a median age of 55 years, but it can also be found in children.
Diffuse primary cutaneous large B-cell lymphoma, leg type (PCDLBCL-LT)
- PCDLBCL-LTT is twice as common in women as in men.
- It has the worst prognosis, with a 5-year survival of 50%.
- It affects older people with a median age of 76 years.
Diffuse primary large B-cell lymphoma, other (PCDLBCL-other)
- PCDLBCL-other is very rare.
- It has a variable prognosis.
What are the cutaneous signs of cutaneous B-cell lymphoma?
Primary cutaneous lymphoma of the follicular center
- PCFCL presents with solive tree or grouped papules, plates or nodules.
- These are pink for violaceous.
- They are usually found on the scalp, forehead, or trunk.
- They are very rarely found on the leg.
Especially when it affects the head or face, PCFCL can simulate rosacea, folliculitis, acne, lupus miliaris (TB), and insect bites. The list of differential diagnoses should also include basal cell carcinoma, Merkel cell carcinoma, cutaneous lymphoid hyperplasia and other non-B-cell skin tumors (eg, cutaneous T-cell lymphomas).
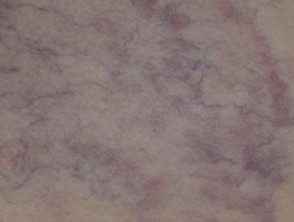
Primary cutaneous B-cell lymphoma of the marginal zone
PCMZL is a low-grade malignant B-cell lymphoma of MALT (mucous membraneassociated lymphoid tissue).
- PCMZL presents with solitary or multiple papules, plaques, or nodules.
- They are red to purplish in color.
- They are most often found on the trunk and upper extremities.
Often the lesions appear clinically minor and, in some case reports, can mimic the appearance of basal cell carcinoma. Other differential diagnoses include arthropod bites urticaria, leukemia skin and drug-induced pseudolymphoma.
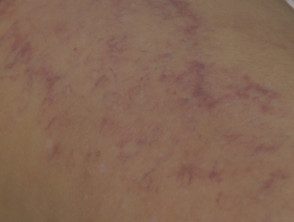
Diffuse primary cutaneous large B-cell lymphoma, leg type
- PCDLBCL-LTT presents with smultiple or olitary nodules, infiltrated plaques and tumors.
- Rarely, it occurs as warty plates o extended garland-like lesions.
- They are typically red to bluish in color.
- They are found mainly on one or both legs, but affects other sites at 10-15%.
- Represents an aggressive subtype of PCBCL.
- Multiple skin lesions on the leg have a poor prognosis.
Diffuse primary cutaneous lymphoma of large B cells, other
- PCDLBCL-other includes large B-cell lymphoma, which presents with skin lesions on the head, trunk, or extremities.
- Blastic plasmacytoid dendritic cell neoplasm it presents with plaques similar to hematomas, nodules and tumors. Later it progresses to involve the central nervous system. It represents a type of leukemia cutis.
-
Intravascular large B-cell lymphoma proliferates within the lumen when I was little blood vessels, mainly in the skin and the central nervous system and later in other organs. Lesions appear as erythematous, sensitive nodules, tumors and telangiectasias mainly on the trunk and lower legs. Skin lesions can be confused with mycosis fungoides, sarcoidosis, blood vessel tumors or leukemia skin.
Intravascular large B-cell lymphoma

Intravascular B-cell lymphoma
Intravascular B-cell lymphoma
Intravascular B-cell lymphoma
How is cutaneous B-cell lymphoma diagnosed?
The evaluation of PCBCLs should include a complete history, a physical exam, and a skin exam. Initial blood tests should include:
- Complete and differential blood count
- Metabolic profile and lactate dehydrogenase.
If the complete blood count shows lymphocytosis, peripheral Blood flow cytometry may be needed.
Adequate skin biopsy It is also important for evaluation and staging. 4–6 mm punch, incisional or excisional biopsies must be obtained and must include the lattice dermis and subcutaneous grease. Surface biopsy samples may not differentiate PCBCLs from reagents or inflammatory processes.
Extracutaneous involvement should be evaluated, especially in patients with palpable lymphadenopathy.
- Contrast Connecticut scan
- PET scan
None lymph node identified on images greater than 1.5 cm in length or showing high PET activity must undergo a biopsy; a excision biopsy preferred wherever possible.
Histologically, PCBCL shows a monotonous diffuse population of centroblasts and immunoblasts. Histochemical tests are essential to classify the exact type of lymphoma.
Primary cutaneous lymphoma of the follicular center
PCFCL needs to be differentiated of a secondary cutaneous lymphoma, which is where a nodal follicular The lymphoma has spread to affect the skin. Cellular morphology may vary with age and size of injury.
Histologically, PCFCL shows:
- Dermal and subcutaneous proliferation of centrocytes (excised follicle core cells) and centroblasts (large transformed cells) in a pattern of follicular and / or diffuse growth.
Immunostaining shows:
- Positive B cell antigensi.e. CD20 and CD79a
- Bcl-2 negative protein, y, t (14; 18) translocation (which if present may suggest systemic follicular lymphoma)
- Negative immunoglobulin M expression.
A FISH Analysis is not useful.
Primary cutaneous B-cell lymphoma of the marginal zone
the histology PCMZL consists of:
- Nodular to spread dermal infiltrators marginal zone B cells, lymphocytes, lymphoplasmocyte cells, plasma cells mixed with reagent T cells and centroblastic or immunoblastic cells
- Marginal zone of B cells, which tend to be small to medium in size with irregular nucleidiscreet nucleoli and abundant pale cytoplasm. They proliferate in the dermal and subcutaneous regions of the skin.
Immunostaining shows
- CD20 positive, CD79a and Bcl-2
- Negative CD10 and Bcl-6.
- Less than 25% from PCMZL harbors the translocation t (14; 18).
- It expresses 150 and 155 microRNAs that, if present, can be predictive of longer progression-free survival.
Primary cutaneous large B-cell lymphoma, leg type
PCFCL and PCDLBCL-LT have diffuse large B-cell infiltrates. PCDLBCL-LT shows:
- Diffuse dermal proliferation of centroblasts and immunoblasts in monotonous or confluent leaves
- Larrge round cores with open chromatinprominent and identifiable nucleoli mitotic figures
- Few T cells confined to perivascular zones
Histopathological Differential diagnoses should include:
- Diffuse large B-cell lymphoma not otherwise specified (DLBCL NOS)
-
DLBCL positive for elderly Epstein-Barr virus
- Lymphomatoid granulomatosis
Immunostaining shows:
- CD20 and CD79a positive with strong expression of cytoplasmic and surface immunoglobulin M.
- Strong expression of Bcl-2, MUM1 / IRF4 and FOX-P1
- Any PCBCL showing expression of Bcl-2 and MUM1 should be classified as a paw type, regardless of anatomical location.
FISH analysis shows translocations of myc, Bcl-6 and immunoglobulin H genes.
What is the treatment for cutaneous B-cell lymphoma?
The rarity of PCBCLs and the lack of prospective randomized comparative studies limit the choice of therapy, as most treatments are based on data from small retrospective studies. The European Organization for Cutaneous Lymphoma Cancer Research and Treatment Group (EORTC-CLG) and the International Society for Cutaneous Lymphoma (ISCL) have uniform recommendations on the treatment of the three main types of PCBCL. Treatment is also influenced by whether the lesion is unique or limited to a single site.
Primary cutaneous lymphoma of the follicular center
Without any treatment, PCFCL lesions may be stable, gradually enlarge, or, rarely, return. the histological Growth pattern does not influence survival or treatment choice.
- If PCFCL presents with a solitary lesion or is confined to a single site, treatment involves radiotherapy or surgery. Recurrences of the skin are common and often outside the treated site, but do not affect the prognosis.
- Radiation can be observed or administered to patients with multiple injuries, current agents, cryotherapy, intralesional steroids or systemic therapy. Where disseminated skin lesions or large tumors occur, chemotherapy may be required, such as CHOP or R-CHOP.
- Immune therapies such as rituximab, interferon, and imiquimod are being explored.
Primary cutaneous B-cell lymphoma of the marginal zone
The recommended therapies for PCMZL are similar to PCFCL.
- Radiotherapy It is highly effective and potentially curative for solitary or few contiguous injuries, but the relapse PCMZL rates may be higher than PCFCL.
- Primary surgery excision can be effective for loners or located PCMZL.
- Local treatments include topical corticosteroids, intralesional steroids, topical nitrogen mustard, intralesional rituximab, and cryotherapy.
- Multifocal skin lesions are treated with chemotherapy agents such as chlorambucil, interferon alfa, and anti-CD20. antibody (rituximab).
- PCMZL associated with Borrelia burdorferi infection can be treated with antibiotics
-
Rarely, disseminated skin lesions are treated with chemotherapy (eg, CHOP).
Primary cutaneous large B-cell lymphoma, leg type
Localized or solitary leg-type B-cell lymphoma is usually treated with local radiation therapy alone or in combination with R-CHOP.
Generalized PCDLBCL-LT can be treated with R-CHOP and / or local radiation therapy. Response rates are high, but relapse rates are> 58% Around 30% they develop extracutaneous disease.
Trials are evaluating the effectiveness of biological agents such as ofatumumab, lumilixumab, dacetuzumab and intralesional TG1042 in the treatment of PCDLBCL-LT.
What is the result for cutaneous B-cell lymphoma?
Primary cutaneous lymphoma of the follicular center
- Solitary or multifocal PCFCL may slowly enlarge or resolve spontaneously.
- Reappearance It occurs in approximately 46.5% of patients.
- The 5-year survival rates are around 95%.
- Dissemination to extracutaneous sites occurs in approximately 5 to 10% of cases.
- PCFCL in the leg has a poorer prognosis with a survival rate of 41% within 5 years.
Primary cutaneous B-cell lymphoma of the marginal zone
- The 5-year disease-specific survival of PCMZL is up to 99%.
- Occasionally, early spontaneous resolution of PCMZL may occur.
- The disease may recur in approximately 40% of patients, especially if multiple sites are involved.
- It is rare that PCMZL metastasis to extracutaneous sites.
Very rarely, PCMZL can be transformed into DLBCL.
Primary cutaneous large B-cell lymphoma, leg type
- PCDLBCL-LT frequently spreads to extracutaneous sites and has a poor prognosis despite aggressive therapy.
- The 5-year survival rates are approximately 50%.
- In a large French multicenter study, leg tumors had a 3-year disease-specific survival rate of 43% versus 77% in PCDLBCL patients who did not affect the leg.
- The 3-year disease-specific survival of patients with multiple skin lesions was 39% compared to 77% in those with single lesions.
Diffuse primary cutaneous lymphoma of large B cells, other
- Large B-cell lymphoma has an excellent prognosis.
- Blast plasmacytoid dendritic cell neoplasia and intravascular large B cell lymphoma have an unfavorable prognosis.

