What is down syndrome?
Down syndrome is common genetic disorder resulting from chromosomal abnormality, trisomy 21. People with Down syndrome have cognitive delay and characteristic features associated with certain medical conditions. [1–8].
Who gets Down syndrome?
the incidence Down syndrome increases with advancing maternal age, but most people with Down syndrome are born to mothers under the age of 30 due to a higher number of pregnancies in this age group. Due to an increase in termination of pregnancies with Down syndrome, live birth predominance it has decreased from one in 700 to about one in 1000 in New Zealand.
Studies suggest marginally higher rates of Down syndrome in boys than in girls.
What causes Down syndrome?
A cell division error during early conception results in three copies of chromosome 21 instead of the usual two. Chromosomal abnormality results from nondisjunction (lack of normal separation) during cell division as the pair of chromosomes both the sperm and the egg do not separate. This results in an additional chromosome 21 gain and the onset of Down syndrome [1–8].
- Standard trisomy 21 is the most common form of Down syndrome (affects 95% in cases).
- Translocation Down syndrome also has three copies of chromosome 21, but one of the 21 chromosomes is attached to another chromosome instead of being separate (affects 3 to 4% of cases).
- Mosaic Down syndrome may be the result of cell division error resulting in two populations of cells within the same individual: one group with 46 normal chromosomes and the other with trisomy 21 (affecting 1-2% of cases).
The clinic phenotype it is similar in all types of Down syndrome, with the subtle differences in mosaic Down syndrome depending on the extent of an individual's population of trisomy 21 cells.
What are the clinical features of Down syndrome?
The diagnosis is suspected or confirmed in the neonatal period in most infants with Down syndrome. The characteristic physical characteristics of Down syndrome include [1–8]:
- Small hands and feet
- Single transverse palm fold
- Associated central hypotonia
- Congenital heart defects
- Gastrointestinal malformations
- Behavioral abnormalities
- Refractive errors (trouble focusing light precisely on the retina due to the shape of the eye)
- Hearing impairment
- Thyroid dysfunction
- Different facial features
- Flat facial profile
- Eyelid tilt up (inner eyelid)
- Low ears
- Brachycephaly (shortened skull).
Cognitive delay is present in all people with Down syndrome. Children are reported to have higher rates of a seizure disorder (8%), celiac disease, and diabetes (1%).
Red blood cells macrocytosis and polycythemia It can affect up to two thirds of babies with Down syndrome. Transient myeloproliferative disorder (TMD), a type of leukemia resulting from trisomy 21, it can be present in up to 10% in newborns. Acute leukemias they are reported in 1 out of 300 individuals with Down syndrome.
Which are the cutaneous characteristics of Down syndrome?
A single transverse palmar fold is the main skin phenotype and is easily detectable. However, a single transverse palmar fold can also occur as a normal variant that is unilateral at 4% and bilateral in 1% of the general population [9–18].
Other skin features include dry skin and a large tongue (macroglossia) with a cracked appearance.
A variety of dermatological disorders are more common in Down syndrome due to a combination of immunity and genetics. deregulation and inefficient physiological processes.
Defective regulation of genes located on chromosome 21 it may play a role in keratosis pilaris, alopecia areata and vitiligo. Immune dysregulation leads to increased susceptibility to bacterial and fungal infections of the skin.
Transient physiological skin manifestations are common during childhood, and chronic Skin conditions appear with age.
Skin characteristics of Down syndrome.

Xerosis

Fissured tongue

Abutment keratosis
What are the cutaneous physiological manifestations of Down syndrome?
Acrocyanosis of hands and feet.
Acrocyanosis is due to poor peripheral circulation and is more pronounced in Down syndrome. It is commonly seen in newborns.
Skin marmorata
Cutis marmorata is a common lace and mottled skin discoloration during early childhood due to impaired blood flow in the small blood vessels Skin Discoloration is most marked on skin exposed to colder ambient temperatures.
Livedo reticularis
The skin change due to reticular livedo is similar but less marked than the marmorata complexion. Livedo reticularis mainly affects the lower extremities, but can also be present in the arms and trunk. It becomes more pronounced in cold climates.
Premature aging
Signs of premature aging reported in Down syndrome include gray hair or thinning of the hairskin atrophyearly development of Ritid (wrinkles), and lentigines. The overexpression of GRASS gene, which regulates free radicals metabolism, is located on chromosome 21 and is overexpressed as a result of trisomy 21; This leads to excess production of hydrogen peroxide, causing the release of cytotoxic hydroxyl radicals. This, in turn, triggers the cell membrane. lipid oxidation, altering the structure and function of the skin and tissues involved.
What are the chronic manifestations of the skin in Down syndrome?
The skin texture is smooth and velvety in infants with Down syndrome compared to unaffected infants. The skin becomes rough with an altered texture during the school years, and most adolescents and adults show chronic skin changes. [9–18].
Chronic skin conditions associated with Down syndrome may be related to immune failure, autoimmune processes, infections and infestationrelated to the disease and defects of keratinization or connective tissue.
Xerosis (Dry Skin)
The skin in Down syndrome becomes increasingly dry, rough and inelastic, and there are irregular spots. lichenification With increasing age.
Eczema or atopic dermatitis
Recent studies report a prevalence of atopic eczema of up to 5%, which is similar to the general population. The eczema patches are red, scalyand itching Generally involve the cheeks, behind the ears, knees and elbow push-ups. Malar erythema It is more commonly seen in Down syndrome than in unaffected individuals. Dry skin predisposes people to irritating contact dermatitis and allergic contact dermatitis.
Seborrheic dermatitis
Seborrheic dermatitis occurs in about a third of people with Down syndrome, often associated with Malassezia folliculitis It presents as a erythematous eruption with yellowish-brown scales involving the scalp, the "T" region of the midface, behind the ears, upper chest, and back
Palmoplantar keratoderma
Palmoplantar keratoderma is thickened skin on the palms and soles of the feet and affects up to 40% in people with Down syndrome. Although rare in infants younger than 5 months, the prevalence of palmoplantar keratoderma is up to 75% for children older than 5 years with Down syndrome.
Abutment keratosis
Keratosis pilaris describes rough spots (which may contain twisted hair) with different red-brown colors. pigmentation. the papules It affects the upper part of the external arms and sometimes the thighs, the external cheeks, the trunk and the buttocks, and occasionally the forearms and legs. Keratosis pilaris usually appears in adolescence for people with Down syndrome.
Pityriasis rubris pilaris
Pityriasis rubra pilaris (PRP) is a rare chronic disease. papulosquamous disorder of unknown cause. It is characterized by well defined areas of hyperkeratotic follicular papules that can evolve into erythroderma. PRP causes thick, smooth, yellow palms and soles and abnormal nail. Immunodeficient states can trigger severe forms of PRP.
Psoriasis
The incidence of psoriasis in the general population is from 1 to 3%; the range is 0.5 to 8% in people with Down syndrome. Immunocompromised patients can develop severe psoriasis.
Syringoma
Syringomas are benign tumors of the eccrine appendices. They are reported in 18 to 39% of people with Down syndrome (up to 30 times more common than in the general population). They are most commonly found in girls and women. Syringomas often develop during adolescence. They are small (0.5–3 mm) flesh-colored or yellow-brown dermal papules and are typically distributed in the periorbital zone.
Milia-I like it idiopathic calcinosis
Cutaneous calcinosis can present as asymptomatic Discreet, firm, small papules, chalk white like milia. These arise mainly in the hands and feet. its Pathogenesis it is not clear. Increased calcium sweat and calcification of the eccrine ducts can contribute, since there is no previous injury or abnormality in calcium metabolism. Calcinosis heals without scarring. the differential diagnosis includes molluscum contagiosum, viral warts, milia, and inclusion cysts.
Elastosis perforans serpiginosa
Serpiginous perforating elastosis (EPS) is rare and affects approximately 1% in patients with Down syndrome. It appears as asymptomatic, erythematous and coalescing from 2 to 5 mm. keratotic papules arranged in linear, arcuateor serpiginous patterns. Papules may have umbilical centers. EPS appears most often on the neck, but it also affects the chin, cheeks, arms, and knees with asymmetric distribution. Lesions develop slowly during adolescence and resolve spontaneously over 6 months to several years, leaving atrophic linear or retinal scars. Generalized EPS is associated with Down syndrome, while the idiopathic form is usually located. EPS can represent a connective tissue dysplasia with transepidermal thickened removal elastic fibers. It is also associated with other connective tissue disorders, such as Ehlers-Danlos syndrome, Marfan syndrome, cutis laxa, elastic pseudoxanthoma, and osteogenesis imperfecta; and it can also be induced by D-penicillamine. The differential diagnosis of EPS includes granuloma annulare, tinea corporis, cancel sarcoidosis, cutaneous calcinosis and Mibelli porokeratosis.
Serpiginous perforating elastosis

Perforating elastosis in Down syndrome
Anetoderma
Anetoderma is a circumscribed area of flaccid skin, often with a fat hernia and an “eyelet” sign on palpation Most often it affects the chest, back, neck and arms. It is usually secondary to elastolysis, which is induced by leukocytes or bacteria associated with chronic folliculitis. The congenital malformation of elastic fibers in Down syndrome can predispose patients to anetoderma.
Oral lesions
Oral injuries are common in people with Down syndrome.
-
The geographic language occurs in approximately 11% of patients with Down syndrome.
- Up to 40% of people with a geographic language also have a fissured language.
- Fissures Red, scaly skin may also appear at the corners of the mouth and lips (angular cheilitis).
- Oral bacterial infection and oral yeast infection can occur.
Angular cheilitis in Down syndrome

Angular cheilitis in Down syndrome
Vitiligo
Vitiligo occurs at any age, with loss of skin pigmentation anywhere on the body. There is a prevalence of 3% for vitiligo in Down syndrome, which is marginally higher than the prevalence of 2% in the general population.
Other pigmentation abnormalities
Other pigmentation abnormalities are common in people with Down syndrome.
- Coffee with milk taint it has an incidence of 4% in Down syndrome, which is similar to the incidence observed in the general population.
- Lumbosacral Dermal melanocytosis is reported more frequently in Down syndrome (seen in 22% compared to 6% in a control group).
- Post-inflammatory Pigmentation is also common in association with lichenified skin.
Alopecia areata
Alopecia areata affects 6-10% in people with Down syndrome compared to prevalence> 2% in the general population.
- Hair loss may persist, but irregular alopecia grows back in most cases.
- Total alopecia or universal alopecia affects up to 2.5% in people with Down syndrome.
-
Trichotillomania can coexist in 2 to 4% of patients with alopecia areata.
- Alopecia areata is associated with autoimmune conditions like vitiligo, hypothyroidismand trachyonychia.
- MX1, the gene for alopecia areata, is assigned to the distal critical region on chromosome 21. The protein of the MxA gene is highly expressed in lesions anagen hair bulbs in alopecia areata, but not under normal conditions follicles.
- Trisomy 21 increases the chance of having the variant alopecia areata gene.
Herpetiform dermatitis
Herpetiform dermatitis is rare. Cause a symmetrical, pruritus, 1–3 mm papulovesicular and erosive rash on the extensor muscle limb, buttock and middle line of the back. Purpuric lesions can be seen on the fingers and toes in children. A celiac examination should be completed if herpetiform dermatitis is suspected. Subepidermal bullas with microabscesses in the dermis papillae, with immunoglobulin To deposit live immunofluorescence, they are confirmatory on the skin biopsy.
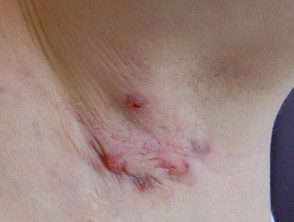
Hidradenitis suppurativa
Hidradenitis suppurativa causes pustules, nodulesand abscesses in the armpits and groin. The response to standard antibiotic treatment is often poor.
Hidradenitis suppurativa in Down syndrome

Hidradenitis suppurativa in Down syndrome
Folliculitis in Down syndrome
Bacterial infections
A variety of bacterial skin infections affect patients with Down syndrome.
-
Folliculitis affects 10% of patients with Down syndrome; this may be due to Malassezia.
-
Furunculosis (boils) and impetigo due to staph infection are common.
Folliculitis in Down syndrome

Folliculitis in Down syndrome
Fungal infections
Ringworm of the foot and onychomycosis are common in Down syndrome.
Dermatophyte infections in Down syndrome

Ringworm of the foot

Ringworm
Parasitic infestations
People with Down syndrome are predisposed to scabies infestations. Crusted scabies can occur in Down syndrome and can be asymptomatic and therefore diagnosed late, which carries a risk of extended infestation in the community.
Lichen nitidus
Lichen nitido causes bright flesh-colored, asymptomatic papules (1–2 mm) distributed in cultures over the genitals, abdomen, trunk, and / or upper extremities in children. the histopathology of lichen nitidus reveals focal papillary dermal lymphohistiocytic infiltrators resembling a "claw" or "baseball glove and ball." The strength of the association with Down syndrome is unknown, but several case reports are cited in the medical literature. [19].
Acanthosis nigricans
Acanthosis nigricans is a marker of insulin resistance and is associated with obesity. It affects the flexions of the neck, the armpitand groin Rarely, it can also affect flexor aspect of the elbow and knee and the dorsal interphalangeal and metacarpal joints
Characteristics associated with obesity in Down syndrome

Acanthosis nigricans

Striae atrophicae
Carotemia
Carotenemia causes a benign yellow-orange tone of the skin that involves the nasolabial folds, outer ears, palms, and soles of the feet, but prevents mucous membranes and sclerotic. It is due to excessive consumption of fruits and vegetables that contain carotenoids, such as carrots and squash, and has been reported in children on food-exclusion diets. allergy [20]. Hypothyroidism associated with Down syndrome can accentuate carotinemia.
Hematological diseases
Rarely, blood disorders such as a transient myeloproliferative disorder or congenital leukemia are reported in babies with Down syndrome.
Leukemia cutis presents as firm, infiltrated, or characteristic blue papules. nodular skin lesions.
How is Down syndrome diagnosed?
The clinical diagnosis of Down syndrome is always confirmed by cytogenetic analysis. A standard or conventional karyotype must be requested A fast fluorescent in the place hybridization (FISH) Analysis of trisomy 21 should be specified on the laboratory request form when an urgent result is required.
After the term, a diagnosis of Down syndrome can be made from the identification of characteristics phenotypic characteristics, but clinical diagnosis is not always possible in patients with mosaic Down syndrome.
Genetic disorders such as Smith-Magenis syndrome, Zellweger syndrome, and Beckwith-Weidemann syndrome can be confused with Down syndrome, as these syndromes present with similar phenotypic characteristics in early childhood.
Careful examination of the skin is required as dermatological problems are reported in up to 87% in people with Down syndrome [9–18].
- Clinical surveillance is required for associated conditions, such as atlantoaxial, obstructive instability Sleep apnea, Celiac disease and diabetes.
- Serum antibody titles and endoscopic Biopsy results indicate a higher incidence of celiac disease in Down syndrome (4.6–7.1%) compared to the general western population (1–2%).
- Routine prenatal Screening and counseling are offered for high-risk pregnancies.
What is the general management of Down syndrome?
Managing the skin and associated medical conditions is important in providing optimal medical care for people with Down syndrome.
- Prenatal Assessment of mothers, diagnosis in the early period of the newborn, regular health surveillance, supervision and support are important.
- Obesity prevention measures are important to avoid skin conditions, musculoskeletal complications, insulin resistance and diabetes.
Other related support services should include:
- Educational and community support.
- Genetic counseling services.
- Prenatal screening during pregnancy
- Chorionic villus biopsy or amniocentesis should be considered early in pregnancy in mothers at risk (see DermNet NZ Prenatal Diagnosis of Inherited Skin Conditions), and pregnancy should be managed with a multidisciplinary team approach.
- The risk of reappearance in a future pregnancy it is slightly higher for the mother with a previous translocation or mosaic Down syndrome.
What is the result for patients with dermatological manifestations of Down syndrome?
Most skin conditions can be managed with optimal care and supervision.
Longevity in people with Down syndrome is influenced by the severity of their birth defects and associated medical problems. Substantial improvements in shelf life are seen with better health surveillance and management compared to a few decades ago.

