What is it hypogonadism in the women?
Hypogonadism in women describes inadequate function of the ovaries, with impaired production of germ cells (ovules) and sex hormonesestrogen and progesterone)
- Primary Hypogonadism refers to a condition of the ovaries (primary ovarian failure / hypergonadotropic hypogonadism).
- Secondary hypogonadism refers to the failure of the hypothalamus or pituitary gland (hypogonadotropic hypogonadism).
What causes hypogonadism in women?
Hypogonadism in women is due to interruption of any section of the hypothalamicPituitary-ovarian axis route (Figure 1). In a working pathway of the hypothalamic-pituitary-ovarian axis:
- The hypothalamus produces the gonadotropin-releasing hormone (GnRH) at the beginning of puberty.
- The GnRH then acts on the pituitary gland, which produces folliclestimulating hormone (FSH) and luteinizing hormone (LH)
- FSH and LH then act on the ovaries to stimulate the production of estrogen and progesterone.
Figure 1. The path of the hypothalamic-pituitary-ovarian axis
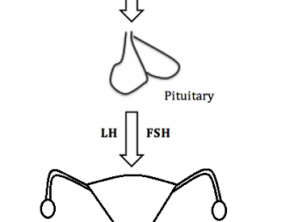
The pathway of the hypothalamic-pituitary-gonadal axis in women
FSH, follicle-stimulated; GnRH, gonadotropin – releasing hormone: LH, luteinizing hormone.
Who gets hypogonadism?
Primary ovarian failure and secondary hypogonadism may be congenital or acquired [1,2].
Congenital primary ovarian failure
The main mechanism for congenital primary ovarian deficiency remains unknown in most cases. Some cases are related to:
- Chromosomal abnormalities like Turner syndrome (45, X karyotype), fragile X syndrome and galactosemia (inability to process galactose sugar)
- Ovarian dysgenesis (abnormal organ development) and agenesis (inability of the organ to develop during embryonic development)
-
Congenital adrenal hyperplasia (17α-hydroxylase deficiency).
Acquired primary ovarian failure
The causes of primary acquired ovarian failure include:
- Medicines, such as chlorambucil, cyclophosphamide, and alkylating agents.
- Radiotherapy
- Autoimmune diseases such as autoimmune polyglandular syndrome type 1
-
Viral infections, including mumps, oophoritis, tuberculosis (TB), malaria, chickenpox, and
- Bacterial infections like Shigella
- Iatrogenic disease, such as problems after oophorectomy (surgical removal of the ovaries).
Secondary congenital hypogonadism
Congenital secondary hypogonadism is gonadotropin deficiency due to a genetic mutation, as in Kallmann syndrome.
Acquired secondary hypogonadism
Acquired secondary hypogonadism may be due to damage to the pituitary / hypothalamus. Causes of acquired secondary hypogonadism may include:
- Intracranial space-occupying lesions (eg, tumors and cysts)
- Infiltrative disease (eg, sarcoidosis and hemochromatosis)
- Infection (e.g, meningitis and TB)
- Pituitary apoplexy (bleeding in the pituitary gland)
- Trauma.
Gonadotropins can be suppressed by:
- Chronic disease (eg, diabetes, anorexia, obesity, and renal disease)
- Excessive exercise
- Critical illness
- Chronic opiates glucocorticoidsor use of anabolic steroids
- Hyperprolactinemia (an excess of the hormone prolactin that induces milk).
What are the clinical characteristics of hypogonadism in women?
The clinical characteristics of hypogonadism depend on the age of presentation. [3].
Estrogen deficiency before puberty
Symptoms of low estrogen levels are rarely present in hypogonadism prior to puberty. Presentation characteristics are absence of pubertal development (reduced growth and absence of pubis hair) and primary amenorrhea (absence of menarche)
Estrogen deficiency after completing puberty.
After puberty is complete, the characteristics of hypogonadism include:
- Secondary amenorrhea (cessation regular periods for 3 months or the cessation of irregular periods for 6 months)
- Symptoms of climacteric (perimenopause): palpitations, heat intolerance, hot flashes, night sweats, irritability, anxiety, depression, sleep disorders, loss of libido, thick hair, vaginal dryness, and fatigue.
- Sterility.
What are the complications of estrogen deficiency?
The long-term risks of estrogen deficiency include an increased risk of osteoporosis and cardiovascular disease. The risk is greater with an earlier age of onset. Conversely, breast risk Cancer can be slightly reduced
What skin changes may be due to hypogonadism in women?
Estrogen plays a key role in maintaining skin health. Estrogen helps maintain skin thickness and collagen levels, skin elasticity and humidity. It is also believed to play a role in wound healing. [4].
Low estrogen levels are associated with:
- Dry and thin skin
- Potentially increased wrinkles
- Delayed wound healing
- Loss of elasticity, thickness and moisture of the vulvar skin, resulting in genitourinary discomfort.
Changes in the skin may also reflect the underlying cause of hypogonadism; for example, hyperpigmentation maybe a sign of an autoimmune disease.
How is hypogonadism diagnosed?
If hypogonadism is suspected after a detailed history and examination, the following avenue of investigation may be followed.
- The patient should be referred to a specialist.
- Initial investigations should include [5,6]:
- Human chorionic gonadotropin (hCG) excludes pregnancy
- FSH and LH
- Estradiol
- Thyroid Stimulating Hormone (TSH): Thyroid disorders can present with amenorrhea
- Serum prolactin
- Pelvic ultrasound exploration: prepuberty.
interpretation of results
- A positive hCG test is due to pregnancy.
- If the uterus is absent or there are other anatomic abnormalities, a karyotype test should be performed.
- Low or low / normal FSH and LH levels may indicate hypogonadotropic hypogonadism. A Magnetic resonance The brain must be considered.
- Before puberty, high FSH and LH levels may indicate primary ovarian failure. Adrenal hormones should be evaluated and a karyotype test should be performed.
- An elevated prolactin result should prompt consideration of a pituitary MRI.
What is the treatment for hypogonadism in women?
Treatment of hypogonadism is directed at the underlying. pathology whenever possible, help women become fertile if desired, and prevent long-term complications of hypoestrogenism (i.e., osteoporosis, increased cardiovascular disease, and urogenital atrophy)
As a general rule, women of reproductive age with hypoestrogenism should receive hormone replacement therapy. The contribution of specialists should be sought, since there are possible significant complications of hormonal therapy, such as:
- Endometrial hyperplasia and carcinoma in unopposed estrogen therapy: it is common to add a progestin to stop this
- Increased risk of breast cancer, venous thromboembolism, stroke and ischemic heart disease.
After menopause, hormone replacement therapy is indicated for significant symptoms.
