What is it anemia?
Anemia (American spelling, anemia) is a deficiency of red blood cells. It can occur through reduced production or increased loss of red blood cells.
Three essential elements must be present to produce red blood cells: iron, vitamin B12, and folic acid. The most common cause of anemia is iron deficiency, which affects more than 2 billion people worldwide.
What is iron deficiency anemia?
The estimate predominance of iron deficiency worldwide is twice that of iron deficiency anemia. Iron deficiency anemia occurs when there is not enough iron to create red blood cells
Who is deficient in iron?
The main groups at risk for iron deficiency and iron deficiency anemia are preschool children, adolescents, pregnant women, and young people, which are times of increased physiological Need for iron.
What causes iron deficiency?
In people living in developing countries, iron deficiency tends to be due to insufficient dietary iron intake or blood loss from intestinal worm colonization. In high-income countries, iron deficiency can result from a vegetarian diet, chronic blood loss or malabsorption.
- Diet-related iron deficiency
-
Malnutrition: poverty, premature babies (milk is a poor source of iron), young children who are fussy
- Strict vegetarian and vegan diets
- Cereal-based diets: decreases the bioavailability of iron, since the phytates in grains reduce iron absorption.
-
- Loss of blood
- Heavy menstruation (periods)
- Gastrointestinal bleeding - from peptide ulcer, polyps or Cancer, can occur over a long period
- Excessive blood donation.
- Gastrointestinal iron deficiency
- Malabsorption
- Crohn's disease
- Helicobacter infection or atrophic gastritis, which can also lead to vitamin B12 deficiency
- Intestinal parasitic infections, such as hookworm or tapeworm
- Medication-related iron deficiency
- Aspirin and nonsteroidal anti-steroidsinflammatory drugs - cause gastritis
- Proton pump inhibitors - may affect iron absorption
- Other conditions
- The pregnancy
- Bleeding disorders, such as von Willebrand disease
- Final stage renal failure: a combination of blood loss from dialysis and low levels of erythropoietin (a hormone that stimulates the production of red blood cells)
- Congestive heart failure, possibly due to subclinical inflammation and impaired iron absorption
- Myelodysplasia: disease of the bone marrow that can present with anemia.
- Intravascular hemolysis (rare) as in paroxysmal nocturnal hemoglobinuria
What are the clinical features of iron deficiency?
The signs and symptoms of an iron deficiency depend on whether the patient is anemic, and if so, how fast does anemia develop. In cases where anemia develops slowly, the patient can often tolerate extremely low concentrations of red blood cells (<100 g >
- Lethargy
- Weakness
- Poor concentration
- Difficulty breathing
- Palpitations
Cutaneous signs of iron deficiency anemia.
The cutaneous signs of anemia are often subtle and may include:
- Pale skin, palm folds, and conjunctiva
-
Angular cheilitis, painful cracks at the corners of the mouth.
- Atrophic glossitistongue loss papillae (smooth and shiny tongue)
- Pruritus and dry skin
-
Nail disorders, including koilonychia
- Dry and brittle hair
- Increased hair loss (telogen effluvium) resulting in diffuse alopecia.
Cutaneous signs of iron deficiency.

Angular cheilitis

Coilonychia
Systemic symptoms of iron deficiency anemia
Other characteristic manifestations of iron deficiency anemia may include:
- Itches: appetite for clay, dirt, paper, or starch.
- Pagofagia: an ice pick, considered quite specific for iron deficiency. Responds quickly to iron replacement.
- Beeturia: excretion of red urine with the consumption of beets. In people with normal iron levels, ferric ions discolor betalaine (red pigment in beets). In iron deficient states, there are inadequate amounts of iron to discolor this pigment.
- Restless legs syndrome - marked leg discomfort that occurs at rest and is relieved by movement.
Iron deficiency can also predispose to bacterial and fungal infections like impetigo, boils and yeast infections.
What tests should be done?
full blood count
A complete or complete blood count (BCF, CBC) is essential to detect anemia. Iron deficiency can be present when blood count rates are normal.
If anemia is due to iron deficiency, the cells are smaller and contain less hemoglobin resulting in a reduced red blood cell count or hematocrit, mean corpuscular volume (MCV) and mean cellular hemoglobin concentration (MCH). The reticulocytic hemoglobin (Ret-Hb) content, which tends to be low in iron deficiency anemia, can be used to control the response to iron replacement. Red blood cells distribution The width (RDW) may reveal a mixed deficiency of iron and vitamin B12 as this results in variable sized red blood cells.
Ferritin
Ferritin is a measure of iron stores and is the most sensitive and specific test for iron deficiency. Low ferritin levels below 15 μg / ml are diagnostic of iron deficiency. Levels above 40 μg / ml in a healthy person are considered optimal.
Normal or high levels of ferritin do not exclude iron deficiency, because ferritin acts as a acute Phase reagent. Levels are higher in the presence of chronic inflammation (eg, Rheumatoid arthritis) when erythrocytes sedimentation rate (ESR) or C-reactive protein (CRP) are elevated. Against the background of inflammation, significantly higher cut-off values are used for ferritin (eg, 100 µg / ml) and are more predictive of iron deficiency. Ferritin is also higher in patients with chronic kidney disease and heart failure.
Other iron tests
In iron deficiency:
- Serum iron is reduced - be aware that serum iron can be highly variable, fluctuate throughout the day, and serum iron is not helpful in evaluating iron stores
- Iron binding capacity is increased - a measure of iron's ability to bind with transferrin (an iron transporter)
- Transferrin saturation is reduced
- Soluble transferrin receiver (sTfR) is reduced: this reflects the total body reserves, except if there is a disease of the bone marrow. sTfR is an expensive test. It is useful to discriminate iron deficiency in difficult cases, for example, in patients with chronic kidney failure or chronic inflammation such as rheumatoid arthritis. It is not modified in anemia of chronic diseases.
Retest iron status after three months of iron supplementation.
Older patients sometimes have unexplained iron deficiency anemia. If intestinal investigation is negative, bone marrow examination may be considered in undifferentiated cases.
What is the treatment for iron deficiency?
Once iron deficiency has been established, the underlying cause should be investigated and managed (correct /control Gastrointestinal bleeding or menstrual blood loss, for example, with the release of levonorgestrel intrauterine device or tranexamic acid for a woman with heavy periods). Most people with iron deficiency anemia will need iron replacement therapy to correct the anemia and replenish iron stores. The benefit of treating iron deficiency without anemia is still uncertain. Specific groups of patients such as those with cardiovascular disease (with heart failure or angina pectoris) should receive red blood cell transfusions that will correct both hypoxia (low oxygen) and iron deficiency.
Increase iron in the diet
Red meat contains heme iron, which is easily absorbed. Non-heme sources of iron may need the help of vitamin C in the form of fresh fruit or tablets.
Many manufactured foods contain iron, so it is essential to read the labels.
Calcium (in dairy products) and tannin in tea, coffee, and red wine reduce the absorption of non-heme iron, so they should be taken several hours before a meal. In contrast, vitamin C (ascorbic acid) improves iron absorption when taken together.
Oral iron
Iron supplementation is safe in pregnancy, infants, children, and adults. It can be used in iron deficiency anemia and anemia of chronic diseases.
Iron preparations come in the form of tablets, oral liquids, and injectables. Oral preparations are the most widely used.
Oral iron preparations from reliable sources include:
- Ferrous fumarate 33% elemental iron
- 20% Ferrous Sulfate Elemental Iron
- Elemental Iron 12% Ferrous Gluconate
Enteric-coated and slow-release formulations are less well absorbed, but better tolerated. Taking iron with vitamin C (ascorbic acid) can increase its absorption and help replenish iron stores more quickly. Lower dose preparations are less effective.
In anemic patients, once hemoglobin levels are corrected within the normal range, iron replacement should be continued for another three months to replenish iron stores. Aim for serum ferritin levels greater than 50 μg / ml.
Iron absorption is reduced in the presence of gastrointestinal disease (atrophic gastritis, infection with Helicobacter pylori, celiac disease, inflammatory bowel disease), chronic kidney disease and inflammatory conditions.
Interactions with iron
Iron can interfere with the absorption of some medications, including:
- Doxycycline
- Fluoroquinolones
- Mycophenolate mofetil
- Penicillamine
- Thyroid hormones.
Iron absorption is decreased by calcium, tannins (in tea and red wine) and vegetable phytates (in cereals). Iron should be taken at a different time of day.
Iron infusions
Intravenous infusions are used in patients who cannot tolerate oral supplementation, or where iron losses exceed the daily amount that can be absorbed orally. Intravenous iron is also essential in the treatment of anemia in patients with chronic kidney disease receiving dialysis and treatment with erythropoiesis stimulating agents (agents to stimulate the production of red blood cells). Parenteral iron in patients with heart failure has led to improvements in physical performance, symptoms, and quality of life.
The most widely used intravenous preparation is polymaltose iron, which is infused over several hours. Other intravenous preparations include low molecular weight of dextran iron, carboxymaltose iron, iron sucrose and ferric gluconate complex.
Side effects of iron replacement.
Adherence to recommended oral iron replacement therapy may be poor in some patients, as iron preparations are associated with high incidence Side Effects These include nausea, constipation, diarrhea, and black stools. To reduce this:
- Take the iron preparation after meals, but the absorption of iron is reduced.
- Wait 30 minutes before going to bed
- Divide the dose and take it twice a day.
- Take it on alternate days, which is better tolerated
- If treatment is not urgent, start with one tablet twice a week and gradually increase dose as tolerated
- Start with doses containing less than 30 mg of elemental iron.
Intravenous polymaltose iron can cause infusion reactions such as headache, nausea, and muscle aches. Serious allergic reactions even anaphylaxis Has been reported. Delayed reactions include fever and joint pain. Extravasation It is rare but may cause persistent brown discoloration of the affected skin.
Intramuscular iron injections are now rarely used. They can cause long-lasting brown spots (siderosis), pain, hematoma and sterile abscesses. An improvement in iron staining has been reported after treatment with Q-Switched ruby and Nd: YAG To be.
Siderosis by iron injection

Intramuscular
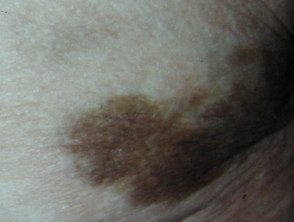
Intramuscular, close-up

Intravenous extravasation
What is the result of iron deficiency anemia?
Most patients with uncomplicated iron deficiency anemia should experience:
- Rapid resolution of pagophagy.
- Better feeling of well-being during the first days of treatment.
- Reticulocyte count (red blood cell precursor) and hemoglobin concentration increased within one week.
- Slow recovery of the papillae from the tongue, skin, nail and hair.
In those who do not respond to treatment, alternative diagnoses should be considered, for example, B12 or folate deficiencies, myelodysplastic syndrome (bone marrow abnormalities), and hereditary anemias.

