What is it discoid lupus erythematosus?
Lupus erythematosus (LE) is a diverse and persistent group. inflammatory autoimmune diseases and often affects the skin. Discoid lupus erythematosus (DLE) is the most common chronic form of cutaneous lupus. It is characterized by persistent scalylike a record plates on the scalp, face and ears that can cause pigmentary changes, scars and hair lost.
What causes discoid lupus erythematosus?
Factors that lead to DLE include:
- Genetic predisposition
- Exposure to sunlight (often several weeks before presentation)
- Toxins like cigarette smoke
- Hormones
The manifestations of DLE are due to the loss of regulation of the immune system in the skin.
Who gets discoid lupus erythematosus?
DLE can affect men and women of any age. DLE is five times more common in women than in men, and the onset is more frequent between the ages of 20 and 40 years. DLE is more common than systemic lupus erythematosus (SLE). The estimate predominance it's around 20 to 40 people out of 100,000.
DLE may be more common in patients with darker-colored skin than in light Caucasians.
DLE is more common and more severe in smokers compared to nonsmokers. Smoking also reduces the effectiveness of antimalarials and other therapies.
Clinical characteristics of discoid lupus erythematosus
Most patients with DLE have only skin involvement (cutaneous LE). Between 5% and 25% of DLE patients develop SLE, in which there may be other forms of cutaneous lupus, and other organs may develop the disease. Systemic symptoms are generally mild in these patients.
DLE can be located (above neck at 80%) or generalized (above and below the neck at 20%).
Signs of localized DLE include:
- Initial injuries are dry red patches.
- These evolve to indurated red o hyperpigmented plates with adherent scale
- Follicular keratosisor plugs curb inside the hair follicles, is observed when the scale is removed from the surface, for example with adhesive tape (tape-tack sign)
- The oldest lesions are hyperpigmented, especially on the edge of the plates.
- Scarring results in a central loss of pigment (white spots) and skin atrophy (tissue loss)
- DLE is usually found in the nose, cheeks, earlobe, and shell
- May involve lips, oral mucous membrane, nose or eyelids
- Scalp injuries cause temporary or permanent patches of hair loss.
- Hypertrophic (wartylupus erythematous describes very thick red plaques.
Signs of generalized DLE include:
- Plates on previous chest, upper back, back of hands
- Sometimes plaques on the upper and lower extremities
- Can affect palms and soles
- Can affect anogenital mucous membrane
The patient's main concern is the unpleasant appearance of the plaques, but they can also cause itching or pain.
Chronic Discoid Lupus Erythematosus (DLE)

Chronic discoid lupus erythematosus
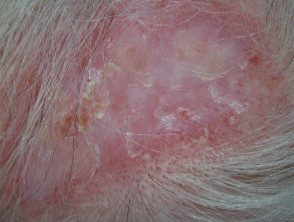
Chronic discoid lupus erythematosus

Chronic discoid lupus erythematosus on the lips
More magicians of cutaneous lupus erythematosus.
How is discoid lupus erythematosus diagnosed?
DLE is often diagnosed by your distribution in places exposed to the sun and the clinical appearance of the plaques. After a careful history, the DLE patient should undergo a comprehensive general examination, to determine if other forms of lupus may be present.
The diagnosis is generally confirmed by the skin. biopsy, in which the typical characteristics of lupus are observed: interface and periadnexal dermatitis, follicular tamponade, atrophy and scarring. Direct immunofluorescence it is often positive on injured skin on DLE (positive lupus band test).
Cutaneous lupus erythematosus disease area and severity index (CLASI)
The severity and area index of cutaneous lupus erythematosus disease (CLASI) was developed in an attempt to classify the severity of cutaneous LE. [2] An activity and disease damage score is calculated at each of the 12 anatomical locations (see original published document for details).
The total activity score is made up of:
- A degree of redness (0–3) and scale (0–2)
- Mucous membrane involvement (0-1)
- Recent hair loss (0–1), no scarring alopecia (0-3).
The total damage score is made up of:
- The degree of dyspigmentation (0–2) and scars (0–2)
- The persistence of depigmentation for more than 12 months doubles the dyspigmentation score.
- Scarring of the scalp (0, 3, 4, 5, 6).
Blood test
Patients with DLE will usually have blood tests at the time of diagnosis and occasionally afterward.
- full blood count
- Renal test run
- Inflammatory markers like C-reactive protein (CRP)
- Antinuclear antibody (ANA, ANF; if present, they generally have a low title)
- Removable nuclear antibody (ENA)
- Anti-annexin 1 antibodies- these may be a diagnostic marker for discoid CLE
Circulating autoantibodies they are found in approximately 50% of DLE patients.
Does discoid lupus erythematosus have any complications?
About 25% of patients with discoid lupus erythematosus also develop systemic lupus erythematosus in the months or decades after the diagnosis of skin disease.
Discoid lupus erythematosus can leave permanent scars, even when the active disease has responded to treatment.
What is the treatment for discoid lupus erythematosus?
Preventive measures
The following measures are important to reduce the possibility of DLE outbreaks.
- Careful year-round protection from sun exposure by wearing broad spectrum clothing, accessories and sunscreens with thick application SPF 50+. Sunscreens alone are not suitable.
- Indoors, some patients may also need to stay away from glass windows, or these may be treated with UV-locking movies.
-
Vitamin D supplements should be recommended for those who strictly avoid the sun.
-
Of smoking cessation.
Current therapy
Intermittent courses of potent topical corticosteroids are the main treatment for DLE. They should be applied precisely to skin lesions for several weeks. The stem should be selected to suit the body site and thickness of the license plate. Very powerful topical steroids can cause thinning of the surrounding skin and increase blood vessel training (telangiectasia) Intralesional corticosteroid injections are sometimes used, especially for hypertrophic DLE.
Calcineurin inhibitors tacrolimus ointment and pimecrolimus cream can also be used.
Camouflage makeup is useful to improve the appearance.
Systemic therapy
Generally, any of the following medications can be used to treat DLE alone or in combination. The treatment is less effective in smokers than in non-smokers.
-
Hydroxychloroquine and other antimalarials: response rates are approximately 80% in CLE.
-
Systemic corticosteroids such as prednisone or prednisolone. They are rarely required for DLE.
-
Methotrexate: better response in subacute CLE and discoid CLE
- Retinoids isotretinoin and acitretin
- Mycophenolate
- Azathioprine
- Dapsone
- Thalidomide
- Belimumab
What is the prognosis for discoid lupus erythematosus?
DLE tends to persist for years or decades. In some patients, all signs of active disease resolve in time.
Scaly cell carcinoma rarely can it arise within a long-standing DLE plate on the skin or mucous membrane. It presents as a warty growth or ulcer. It is usually treated surgically.

