What is peanuts? allergy?
Peanut allergy is an adverse immune response to a peanut allergen. Reactions include:
- Systemic immunoglobulin E (IgE) mediated by immediate type I hypersensitivity reaction (anaphylaxis) [1]
-
Oral allergy syndrome - a located IgE-mediated allergy caused by fresh fruits, vegetables and nuts, with symptoms limited to the lips, mouth, and throat [2]
- Non-IgE-mediated allergy: This response can take hours to days to occur and produces gastrointestinal symptoms (vomiting, diarrhea, and abdominal pain) [1].
Peanut allergy is the most common food-related cause of anaphylaxis. [3].
Misery

What are the peanuts Allergens?
PeanutsArachis hypogaea) belongs to the legume family and is distinct from the dried fruit family.
There are 11 peanut allergens (Ara h 1 to Ara h 11); These allergens are seed storage proteins and biological reserves that allow the peanut seed to grow into a plant.
Who gets a peanut allergy?
In the UK, the predominance allergy to peanuts is reported to be 0.2 to 2.5% in children and 0.3 to 0.5% in adults [4,5]. An increase in prevalence was reported in the United States, with 1.4% in children with peanut allergy in 2008 compared to 0.4% in 1997 [6].
There is an increased risk of peanut allergy in children who have:
- Egg allergy
- Serious atopic dermatitis
- Used current preparations containing peanut oil.
Having a peanut allergy does not increase your risk of allergy to another legume (for example, peas, beans, lentils, and soybeans) with the exception of lupine. However, a third of people with a peanut allergy will have a concurrent reaction to a tree nut (eg, walnut, almond, Brazil nut, and coconut) [7].
Peanut allergy is more predominant in the western world than in China, possibly due to the higher consumption of roasted peanuts rather than raw peanuts [8].
The Learning Early About Peanut Allergy (LEAP) study found that infants at risk of peanut allergy who have eczema or an egg allergy were less likely to develop a peanut allergy if they had early and sustained peanut consumption [9].
Non-allergic mothers are now encouraged to potentially eat allergenic foods such as peanuts regularly during pregnancy and do not delay the presentation of their babies [10].
What Causes Peanut Allergy?
The cause of peanut allergy is not fully understood.
- Peanuts are highly allergenic due to the abundance of allergens in seed storage proteins.
- Peanuts are highly resistant to enzymatic digestion when it is in the gastrointestinal tract, and its allergens maintain their conformational epitope structure (a three-dimensional folded polypeptide). Most IgE bind to the Ara h 2 conformational epitopes; An allergic immune response can be invoked when IgE binds to a peanut allergen.
- Dendritic cells they have specific receptors to identify carbohydrate residues. the Carbohydrate residues on the surface of peanuts can activate dendritic cells and invoke an allergic immune response.
- When peanuts are roasted, they undergo a non-enzymatic glycosylation reaction called the Maillard reaction. This alters the structure of the amino acids and sugars in peanuts, and makes the peanut more allergenic [11].
To develop a peanut allergy, the individual must be exposed to one of the peanut allergens through a gastrointestinal system, cutaneousor airway.
- The peanut allergen is detected by a dendritic cell, which moves to a lymph node to interact with a specific T cell receiver. In abundance of interleukin (IL) -4, IL-5 and IL-13, a T-helper type 2 (TH2) cellular response is initiated.
- TH2 response signals B cells to produce specific allergens clone IgE IgE binds to the high affinity IgE receptor (FcεRI) on the surface of mast cells. The expression of FcεRI in mast cells is up-regulated (increased) so that more IgE can bind to the mast cells (leading to allergic priming or sensitization)
- When the individual is subsequently exposed to the peanut allergen, the allergen can immediately bind to IgE on the surface of mast cells, causing an allergic response. The mast cell degranulates and releases various chemicals, including histamine, what causes vasodilation, increased vascular permeability, and the clinical signs and symptoms of a allergic reaction.
- In non-allergic individuals, T regulatory cells lead to tolerance to the peanut allergen [11].
What are the clinical features of peanut allergy?
Peanut allergy results in urticaria, angioedemaand anaphylaxis within 30 minutes of exposure to a peanut allergen [1]. It can also cause a late-phase allergic reaction.
Anaphylaxis causes dyspnea (dyspnea) and wheezing (due to bronchospasm and laryngeal edema), tachycardia, hypotension, dizziness and loss of consciousness. Anaphylaxis is a life-threatening clinical emergency. [1].
A late-phase allergic reaction can develop 2 to 6 hours after initial exposure to the allergen and peaks around 6 to 9 hours. This is due to the recruitment of leukocytes and antigen-specific T cells. The late phase reaction results in erythema and edema, sneezing, itching, and coughing. It usually resolves completely in 1 to 2 days. [12,13].
What are the complications of peanut allergy?
Anaphylaxis can be fatal if it is not recognized and treated promptly with adrenaline, a bronchodilator, and antihistamines.
Children with asthma have a higher mortality from peanut-induced anaphylaxis than non-asthmatic children. [14].
How is a peanut allergy diagnosed?
Peanut allergy is primarily a clinical diagnosis based on the rapid development of allergic symptoms and signs after eating a peanut.
Skin prick test and serum Specific IgE tests are used to identify sensitization and confirm the diagnosis. [4].
The skin prick test involves placing a drop of peanut allergen on the skin, then pricking the skin to see if bump Produces in 15 minutes. The British Allergy Society and Clinic Immunology (BSACI) states that a scarring ≥ 8 mm in size is highly predictive of peanut allergy. The skin prick test should be performed in a specialized center with emergency kits available in case of anaphylaxis. [4].
The serum specific IgE test, also known as a radioallergosorbent test (RAST), is performed to detect allergen-specific IgE in the blood. Specific IgE ≥ 15 kU / L is highly predictive of peanut allergy [4].
These tests do not predict the severity of the clinical allergy. [4].
Which is the differential diagnosis for peanut allergy?
An IgE-mediated type I hypersensitivity reaction and subsequent anaphylaxis may be due to other causes. For example:
- Other food allergies (such as egg, milk, wheat, soy, and sesame seeds)
- A drug known to cause anaphylaxis (such as an antibiotic or non-steroidal anti- steroid).inflammatory drug)
- Exercise-induced anaphylaxis
- Food-dependent exercise-induced anaphylaxis (most often due to peanuts, wheat, shellfish, tomatoes, or corn)
-
Allergy to bee and wasp stings.
The sudden development of a eruption it could be due to the non-allergic release of histamine, as in scombroid fish poisoning.
What is the treatment for a peanut allergy?
Treatment of anaphylaxis is a medical emergency that involves stabilization of the airways, breathing, and circulation.
- Intramuscular epinephrine (epinephrine) should be administered immediately to patients with signs of shock, swelling of the airways, or definite difficulty in breathing.
- This can be followed by treatment with an antihistamine, a corticosteroid, and other drugs.
Confirmed peanut allergy needs a comprehensive management plan, which should be shared with the patient's wider family, school, and / or workplace. [4,15,16].
Anaphylaxis treatment
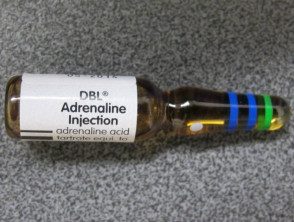
Adrenaline injection

Antihistamine tablets
Avoid nuts
The patient should completely avoid the consumption or touch of peanuts, peanut butter, peanut flour, arachis oil, and other products that contain peanuts. Ingredient lists and warnings on manufactured foods should be read (in New Zealand, the US and many other countries, the possibility that an item containing peanuts may need to be declared on the package). Patients should be especially careful when eating out, where unintentional contamination of other foods with peanuts can occur.
It is not clear whether peanut allergy patients should also avoid all legumes and nuts.
- If a specific type of legume or nut has been previously tolerated, it should be safe to continue eating it.
- If the legume or walnut has not been tested before, it is safer to assume allergy to it [4].
Prepare for an allergic reaction.
Antihistamines should be carried at all times and taken if an allergic reaction occurs. The patient and their caregivers should be regularly trained on how to use an epinephrine or adrenaline autoinjector in a prepared syringe, and if the device is to be used, the patient should seek immediate medical attention. [4].
Test family members for peanut allergy
Between 5% and 9% the siblings of children with a peanut allergy will also have a peanut allergy. In individuals at high risk for an allergic reaction (those with asthma, eczema, or other foods allergies) or in cases of parental anxiety, it is advisable to carry out skin prick tests or specific IgE tests before the child introduces peanuts into his diet. In individuals at low risk of allergy, peanuts can be carefully introduced to detect an allergic reaction [4].
Immunotherapy
Oral clinical trials, sublingual, and epicutaneous peanut immunotherapy has shown some promising results, but at present, this is not routinely offered as a treatment for peanut allergy [4].
Humanized anti-IgE monoclonal antibody Omalizumab therapy has been shown to accelerate desensitization in peanut immunotherapy [17].
What is the result of peanut allergy?
About 20% of children with allergies will grow from peanut allergy [10]. The allergy persists into adult life in most affected people.

