What is a systemic corticosteroids?
A systemic corticosteroid (or "steroid") is a medication derived from cortisol, a natural steroid produced by the adrenal gland in the body. Systemic steroids are prescribed in dermatology for inflammatory skin diseases, such as:
- Eczema/ /dermatitis
- Autoimmune bullous diseases
- Lupus erythematosus
- Sarcoidosis
- Cutaneous vasculitis.
Skin diseases treated with systemic corticosteroids.
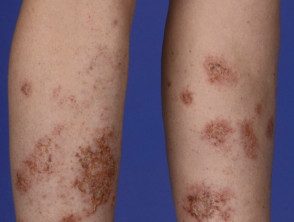
Discoid eczema

Bullous pemphigoid

Cutaneous vasculitis
Risks of Long-Term Systemic Corticosteroid Use
There are risks from the long-term effects of systemic steroid therapy, including infections (bacterial, fungal and viral), hypertension, diabetes, osteoporosis, avascular necrosis, myopathyand glaucoma.
There are several ways that some of these risk factors can be reduced, including through ongoing assessment and monitoring, lifestyle changes, and prophylactic deals.
The risks detailed below refer to patients treated with > 7.5 mg/day of prednisone (or equivalent doses of other corticosteroids) for periods of time greater than 3 months. Below these levels, the risk of health effects is negligible.
Effects on bone health.
Systemic steroids stimulate bone resorption (breakdown) and reduce bone formation in the first few months of starting treatment, increasing the risk of osteoporosis and fracture. [1,2].
Evaluations
An assessment of bone mineral density (BMD) at the lumbar spine and/or hip should be performed at initiation of systemic steroids.
Consider a fall assessment for those at increased risk for falls.
Blood tests aren't usually needed, but they can check for:
- Vitamin D levels, using a 25-hydroxy vitamin D blood test (aiming for >50 ng/mL)
- Calcium levels.
lifestyle tips
The risk of developing osteoporosis can be reduced by implementing lifestyle changes. These include:
- The introduction of weight-bearing and bone-loading exercises
-
Of smoking cessation
- A diet rich in calcium.
- Avoid excessive alcohol consumption (> 3 standard drinks / day is detrimental to bone health); The recommendations of the New Zealand Ministry of Health are as follows:
- Women: 2 standard drinks / day, <10 bebidas estándar >
- Men: 3 standard drinks / day, <15 bebidas estándar >
- At least 2 days without alcohol per week [3].
Osteoporosis prevention
The prevention of osteoporosis is controversial. A bisphosphonate (eg, alendronic acid, risedronate sodium, or zoledronic acid) is first-line therapy if the T-score measured by BMD is <-1 (es decir, que muestra osteopenia o baja masa ósea) [4,5]. La osteoporosis es un puntaje T de <−2.5.
Bisphosphonates are also recommended for patients taking ≥ 7.5 mg/day of prednisone (or equivalent) for a duration of ≥ 3 months if they fall into the following categories [4,5]:
- Postmenopausal women and men ≥ 50 years.
- Premenopausal women and men <50 años con antecedentes de fragility fracture.
Other options for osteoporosis
- Calcium carbonate supplementation (1000–1500 mg/day) is recommended only if intake is inadequate through diet [1,5].
- Vitamin D3 supplementation (800 IU/day) is recommended in those with very little skin exposure to sunlight (see Vitamin D).
- Calcitonin is a second-line therapy on specialist advice and may be recommended if bisphosphonates are not suitable or if the patient has had a acute fracture (reduces bone pain) [1].
- parathyroid hormone analog term (teriparatide 10 mg/day) is often used in the treatment of osteoporosis instead of prophylaxis.
- Hormone replacement may be recommended for premenopausal women with menstrual irregularities, but data for its use in postmenopausal women are insufficient to recommend it for prophylactic use. [5–7].
Prevention of osteoporosis in children.
There are currently no evidence-based guidelines for the prevention and treatment of steroid-induced osteoporosis in children. Currently experts recommend [4]:
- proper nutrition
- Maintaining a healthy weight.
- Promotion of exercise with weights
- Vitamin D supplementation to achieve at least 50 nmol/L, ideally 75 nmol/L (if measured)
- Calcium supplements (if diet is inadequate)
- Long-term safety data on the use of bisphosphonates in children are still required; however, they are currently recommended by experts for use in children with evident bone fragility and reduced BMD.
heart disease
Systemic steroid use is associated with hypertension, hyperglycemia and obesity, which are risk factors for ischemic heart disease and heart failure.
Evaluations
Assess the patient's current risk factors for cardiovascular disease (CVD); this will include assessing:
- Blood pressure
- Cholesterol levels
- Physical activity levels and diet.
- Any family history of CVD, type 2 diabetes and genetic lipid disorders
- The patient's previous medical history, including heart attacks, strokes, atrial fibrillation, or renal disability
-
smoking status
-
Diabetes/blood status glucose levels:
- Quick plasma glucose 4–7 mmol/L recommended
- 2-hour plasma glucose 5–10 mmol/L is recommended.
lifestyle tips
The risk of the patient developing CVD can be reduced by the following lifestyle factors:
- Diet:
- Restriction of sodium intake
- Eat foods rich in potassium (eg, broccoli, carrots, fish, and poultry)
- Eat a diet high in fiber and whole grains.
- Reduction of cholesterol intake.
- Weight loss if necessary (calculate body mass index)
- Eat a diet low in saturated fat [8]
- Give up smoking
- Physical activity; aspire to:
- 2.5 hours of moderate intensity per week OR
- 1.25 hours of vigorous intensity per week [8].
Prevention of cardiovascular diseases.
Calculate the patient's cardiovascular risk. If the result of your calculations presents your risk as:
- Bass: promote lifestyle changes
- Moderate– Discuss the benefits and harms of blood pressure and/or lipid-lowering medications, and lifestyle changes
- High: Discuss with these patients how they are likely to benefit from blood pressure and lipid-lowering medications, as well as antiplatelet medications, and intensive lifestyle interventions. Recipes may include:
-
Antiplatelet therapy (aspirin)
- Statins (hypolipidemics)
- Thiazide diuretics: reduce hypertension and long-term risk of osteoporosis [1].
- Aim for the following goals with patients at high risk for CVD:
- Blood pressure <130>
- Low-density lipoprotein cholesterol <2.0 mmol / L.
Evaluate the lipid profile of the patient in base, after 1 month, and then every 6–12 months after initiation of systemic steroids. The Framingham Risk Score can be used to assess an individual's 10-year risk of developing CVD, and can be used to guide treatment [4].
hyperglycemia
Systemic steroid use has effects on glucose levels within hours, and is associated with hyperglycemia and insulin resistance [4].
Evaluation
Assess the patient's blood glucose levels. The recommended ranges are:
- Fasting plasma glucose: 4–7 mmol/L
- 2-hour plasma glucose: 5–10 mmol/L.
glycosylated hemoglobin (HbA1 C) is a measure of blood glucose over the previous 3 months. HbA level1 C indicates the risk of diabetes:
- <40 mmol >
- 40–50 mmol/mol: insulin resistance or “pre-diabetes”
- > 50 mmol/mol: diabetes.
Treatment of hyperglycemia.
If blood glucose levels are not within normal ranges, initial management should be implementation of lifestyle modification strategies as described for CVD. If blood glucose goals are not met, glucose-lowering medications are recommended.
Random plasma glucose > 11 and <15 mmol >
- Metformin
- Dipeptidyl peptidase-4 inhibitors
- Sulfonylureas: Sulfonylureas with a short half-life (eg, gliclazide) are suitable for patients on prednisone once daily; Drugs with longer half-lives (eg, gliclazide modified-release) are suitable for those with shorter-acting steroids given more than once daily.
- similar to glucagon peptide-1.
If blood glucose levels are >15 mmol/L, insulin may be required to control glycemia.
Steroid-induced diabetes in children will require the advice of a multidisciplinary physician. pediatric diabetes health care team. Lifestyle interventions are first-line therapy, followed by insulin [4].
Gastrointestinal disease
Systemic corticosteroids may cause an increased risk of gastrointestinal events, such as gastritis, peptide ulcerand gastrointestinal hemorrhage [1,4].
Evaluation
Assess the patient's history for peptic ulcer risk factors [5]; These include:
- NSAID use (increases peptic ulcer incidence quadruple)
- Of smoking
- Helicobacter pylori infection
-
alcohol use
- Age> 65 years
- Current or previous peptic ulcer disease
- Serious comorbidities, such as advanced. Cancer.
Prevention of gastrointestinal diseases.
After a thorough evaluation, if you believe a patient is at high risk for GI disease, consider prescribing an H2receiver antagonist or a proton pump inhibitor [4].
Immunosuppression
El uso de esteroides sistémicos afecta directamente immune cells, como T-lymphocytes, y el sistema inmunitario no puede responder a la infección de manera tan efectiva como lo normal, lo que aumenta el riesgo de infección [4].
Anime al paciente a presentarse temprano si no se encuentra bien.
Evaluation
Lleve un historial de vacunación que cubra las vacunas de rutina para niños y adultos del paciente antes de iniciar la terapia; las vacunas de rutina incluyen [9]:
- Vacuna contra la influenza
- Hepatitis A y B
- Rotavirus
- Difteria, tétanos y tos ferina
- Haemophilus influenzae tipo b
- Human papilloma virus
- Herpes zoster (shingles)
- Neumococo
-
El sarampión, las paperas y la rubéola.
Cualquier prueba para chronic la infección debe incluir:
-
Virus de hepatitis B y virus de hepatitis C serology
- HIV serology
-
Examen de detección de tuberculosis, utilizando un análisis de piel derivado de proteína purificada (PPD) o análisis de sangre QuantiFERON Gold [5].
prevent infections
La infección se puede minimizar mediante el lavado frecuente de manos, evitando la exposición a otras personas con infección y el uso de vacunas apropiadas.
Administre las vacunas faltantes o indicadas antes de iniciar la terapia con esteroides sistémicos. Administre vacunas vivas al menos 2 a 4 semanas antes, ya que los esteroides sistémicos reducen effectiveness y aumentar el riesgo asociado con las vacunas [5].
Necrosis avascular
La necrosis avascular ocurre cuando hay pérdida de flujo sanguíneo al hueso, lo que lleva a heart attack del hueso, a menudo en la cabeza femoral. El riesgo de desarrollar osteonecrosis aumenta con el aumento de las dosis de corticosteroides sistémicos. [5].
Evaluation
Evaluar el historial médico previo del paciente para determinar los factores de riesgo de necrosis avascular; Los factores de riesgo incluyen:
- Hemoglobinopatías de células falciformes
- Systemic lupus erythematosus
- Renal transplant
- Gout
- HIV infection
- Hipercoagulable estados
- Trauma
-
Antiphospholipid antibodies.
Pregunte sobre el consumo de alcohol del paciente, ya que esto puede aumentar el riesgo de necrosis avascular. Recomiende que eviten el consumo excesivo de alcohol.
Monitoree de cerca a los pacientes con un riesgo elevado de necrosis avascular.
Supervision
Controle cualquier dolor articular y el rango de movimiento de la articulación, ya que el diagnóstico temprano y la intervención adecuada pueden prevenir o retrasar la progresión de la necrosis avascular. [1].
Si se sospecha necrosis avascular, puede diagnosticar usando:
- A Magnetic resonance de la articulación afectada [1,5]
- Remisión a reumatología si se trata [1].
Treatment of avascular necrosis.
El tratamiento de la necrosis avascular implica inicialmente:
- Actividades de carga parcial
- Bed rest
- Analgésicos para aliviar el dolor.
Si el tratamiento conservador falla, se pueden considerar opciones adicionales, como la cirugía [1].
Cambios conductuales y cognitivos.
El uso de esteroides sistémicos puede alterar el estado de ánimo del paciente o causar déficit de memoria, agitación, ansiedad, letargo y psicosis. [1,4].
Evaluation
El paciente debe ser evaluado por cualquiera de los siguientes factores de riesgo:
- Antecedentes familiares de depresión o alcoholismo.
- Systemic lupus erythematosus
- Preexisting psychiatric disorders
Bass serum Los niveles de albúmina predicen la psicosis en pacientes con lupus eritematoso sistémico. [1,4].
Monitoree cualquier cambio en el comportamiento o estado cognitivo del paciente.
Treatment of behavioral disorders.
El carbonato de litio se puede usar como profilaxis para la psicosis en aquellos pacientes que están predispuestos a la psicosis. [1,4].
Los síntomas persistentes de psicosis pueden indicar que se requiere terapia antipsicótica. La mayoría de los pacientes se recuperan con reducciones de dosis o con el cese de los esteroides sistémicos.
Si un paciente experimenta alteraciones del sueño y sueños desagradables, considere cambiar su dosis de esteroides sistémicos a una sola dosis matutina, o administre medicamentos con efectos sedantes por la noche. [4].

