
Ad
Skin cancer
Application to facilitate skin self-examination and early detection. read more.
Introduction
Melanoma of the nail unit is usually a variant of acral Lentiginous melanoma (melanoma that arises on the palms of the hands and the soles of the feet). Other types of melanoma rarely arise under the nail They are nodular melanoma and desmoplastic melanoma.
Melanoma of the nail unit usually affects one toenail or one large toenail, but any finger or toenail may be involved. The term includes:
- Subungual melanoma (melanoma originating from the nail matrix)
- Ungual melanoma (melanoma that originates under the nail plate)
- Periungual melanoma (melanoma originating from the skin next to the nail plate)
Who gets melanoma from the nail unit?
Nail unit melanoma is rare, representing only about 1% of melanoma in white-skinned individuals. It arises in people of all races, whatever their skin color. Although not more common on dark skin than light skin, it is the most common type of melanoma diagnosed in depth. pigmented individuals. It is most commonly diagnosed between the ages of 40 and 70. [one].
It is not believed to be due to sun exposure. Trauma can be a factor, which represents the largest incidence on the big toe and thumb.
Melanoma management is evolving. For updated recommendations, see the Australian publication. Cancer Council clinical practice guidelines for the diagnosis and management of melanoma
What does the melanoma of the nail unit look like?
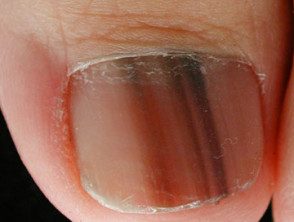
Subungual melanoma often begins as a pigmented band visible along the nail plate (melanonychia) For weeks or months, the pigment band:
- It becomes wider, especially in its proximal extreme (cuticle)
- It becomes more irregular in pigmentation including light brown, dark brown
- It extends to involve the skin of the adjacent proximal or side nail fold (Hutchinson sign)
- You can develop a noduleulcerate or bleed
- May cause thinning, cracking, or distortion of the nail plate (nail dystrophy)
However, in up to half of all cases, subungual melanoma is amelanotic (unpigmented) Megal melanoma can form a nodule under the nail plate, lifting it up (onycholysis) Sometimes it can look like a wart (warty) It is usually painless, but an advance tumor invading the underlying bone can cause severe pain.
A melanocytic nevus of the nail matrix results in a pigmented band (melanonychia). This tends to be narrower than 3mm (but can be wider) and a uniform brown or dark brown color. Benign The pigmentation seen in the cuticle or proximal nail fold is known as a pseudo-Hutchinson sign.
Melanoma of the nail unit
Melanoma of the nail unit

Melanoma of the nail unit

Melanoma of the nail unit
See more images of melanoma of the nail unit.
How is melanoma of the nail unit diagnosed?
Subungual melanoma can be clinically suspected due to a wide (> 3 mm) band of new or changing pigment in a single nail. Dermoscopic examination may reveal more details showing pigmented lines of different colors, width and spacing. These lines tend to lose their usual tendency to run parallel to each other across the nail. Ungual melanoma forms an unpigmented lump under the nail plate, ultimately resulting in its destruction.
The diagnosis of melanoma is confirmed by biopsy of the nail matrix and the nail bed. It can be a difficult diagnosis that requires examination by expert dermatopathologists. the pathologist you must report whether the melanoma is in the place or invader. The description of invasive melanoma should include its thickness in millimeters and what level of tissue has been invaded.
If the clinical diagnosis is subungual hematoma (a purple mark under the nail due to bleeding or bruising), the nail may be seen for a few weeks. The normal looking nail should be seen to grow behind the mark. Dermoscopy is useful since the hematoma does not conform to the band pattern of subungual melanoma. However, it must be remembered that melanoma can bleed.
Other diagnoses that are often considered include onychomycosis (fungi infection), paronychia, pyogenic granuloma and scaly cell carcinoma. See also subungual melanoma. pathology.
Algorithms for the diagnosis of melanoma of the nail unit
ABCD criteria for subungual melanoma in the place
Lee et al have suggested ABCD nail criteria to diagnose subungual melanoma in situ when a patient presents with longitudinal melanonychia. The diagnosis was confirmed in his 26 patients with subungual melanoma in situ and 28 patients with nail matrix. naevi [2].
- A - adulthood (age> 18 years)
- B - brown bands on a brown background
- C - periungual skin color
- Done digit.
ABCDEF Guidelines for Pigmented Nail Injury
Levit et al described the ABCDEF guidelines for evaluating pigmented nail lesions [3].
- A: age 40–70 years old; African, Japanese, Chinese, and Native American heritage
- B: brown-black band ≥ 3 mm with variegated edges
- C: change or lack of change in the band of the nail or the nail morphology
- D: Most commonly involved digit (thumb, big toe, or index finger)
- E: extent of discoloration in the skin surrounding the nail (Hutchinson's sign)
- F: family or personal history of melanoma
Dermoscopic tracks to differentiate pigmented nail bands
In the International Dermoscopy Society survey evaluating dermoscopic tracks in pigmented nail bands, melanoma cases were significantly associated with [4]:
- The width of the pigmented band that occupies more than two thirds of the nail plate.
- Gray and black colors
- Irregularly pigmented lines
- Hutchinson's sign and micro-Hutchinson's sign (skin pigmentation seen on dermoscopy but not on clinical examination)
- Nail dystrophy.
Granular pigmentation, a recently defined dermoscopic criterion, was found in the 40% of melanomas and only in the 3,51% of benign lesions. The dermoscopic feature of any pigmentation in hyponychia (the distal finger pulp under the nail plate) are parallel pigmented lines on the ridges (in contrast to nevi where pigmentation affects the grooves or may be diffuse)
What is the treatment of melanoma of the nail unit?
Melanoma must be removed surgically. This requires removal of the entire nail apparatus. Sometimes the end of the toe or toe is amputated.
Some patients may be offered a sentinel node biopsy to determine if the melanoma has spread to the local lymph nodes.
What is the prognosis for melanoma patients who affect the nail unit?
The main factor associated with the risk of melanoma spread (metastasis) and death is the thickness of the melanoma at the time of completion excision of the primary tumor. Delayed diagnosis is common with subungual melanoma, particularly when it affects the toe, and some of these tumors have already spread at the time of diagnosis.
The 5-year survival rate varies widely from 16% to 87%, depending on the series, with two larger series in the range of 51% to 55% [5].

