Introduction
Adalimumab belongs to a class of biological medicines called tumor necrosis factor blockers (TNF). It is approved in adults and children over 4 years of age for the treatment of psoriatic psoriasis. arthritispolyarticular youth idiopathic arthritis, ankylosing spondylitis, rheumatoid arthritis, ulcerative colitis and Crohn's disease, and uveitis. In September 2015, the FDA also approved adalimumab for the treatment of hidradenitis suppurativa. In New Zealand (October 2019), PHARMAC has approved funding on the application of the Special Authority in certain circumstances for severe psoriasis resistant to treatment, hydradenitis suppurativa moderate to severe, Behcet syndrome and pyoderma gangrenous
The original brand of adalimumab has the brand name Humira®. Generic biosimilar adalimumab is also available in several countries.
How effective is adalimumab in psoriasis?
Adalimumab has been studied in several thousand adult patients with moderate to severe psoriasis. the effectiveness of the medication was judged using PASI (Psoriasis area and severity index) before treatment and after using adalimumab 40 mg every 2 weeks. More than 70% of the patients achieved a reduction of 75% in the PASI score at 16 weeks, and in the 15-20%, the psoriasis disappeared completely.
Adalimumab is not a cure for psoriasis and should be continued in the long term. Although it continues to be effective in most patients, psoriasis sometimes recurs despite continued injections of adalimumab. This is called a secondary failure.
Adalimumab 40 mg every 2 weeks has also been studied in several hundred patients with psoriatic arthritis. Most patients experience some improvement in joint pain and swelling in at least some affected joints, and some patients report a notable benefit of treatment.
Psoriasis before and 6 months after starting adalimumab

Psoriasis before starting adalimumab

Psoriasis before starting adalimumab

Psoriasis before starting adalimumab
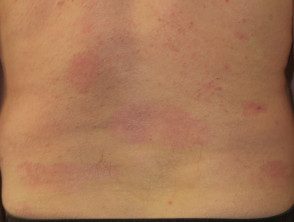
Psoriasis 6 months after starting adalimumab

Psoriasis 6 months after starting adalimumab

Psoriasis 6 months after starting adalimumab
See more images of psoriasis treated with adalimumab.
How does adalimumab work?
Adalimumab is a recombinant monoclonal antibody containing only humans peptides. It works by directly joining the TNF molecules in the blood and diseased tissue. TNF bound to adalimumab cannot cause inflammation which results in psoriasis plates.
Adalimumab is also effective for others. inflammatory Skin diseases; It is registered for the treatment of Hidradenitis suppurativa. In New Zealand, it is funded to treat some cases of Behçet gangrenous disease and pyoderma.
How is adalimumab given?
Adalimumab is administered by subcutaneous injection once every two weeks. It is available as a pre-prepared syringe or pen. After initial counseling and training, patients can usually self-inject into the thigh or abdomen. A different site should be used with each injection to reduce pain and prevent the skin from becoming tender, red, bruised, or hard.
Adalimumab treatment

Remove the pen caps

Giving the subcutaneous injection

Pressing at the injection site
The recommended dose to treat psoriasis is 80 mg and then 40 mg a week later, followed by 40 mg every two weeks as a single dose.
Other medications, including methotrexate and acitretin, can generally be continued during treatment with adalimumab.
Pretests for adalimumab
Dermatologists are likely to request a routine blood count, liver, and renal function, fast lipids and antinuclear antibody (ANA) before starting adalimumab. In women, a pregnancy test may be appropriate.
Patients should be examined for tuberculosis (TB), active or latent viral hepatitis (HAV, HBV, HCV) and the human immunodeficiency virus (HIV) If present, these infections should be treated before starting adalimumab.
Vaccines and adalimumab
Immunization status should be reviewed before starting adalimumab. If necessary, vaccines should be updated before treatment. Annual influenza vaccination is recommended.
Because they can induce disease in immunodeficient individuals, live vaccines should not be used during treatment with adalimumab. Currently, available live attenuated viral vaccines include measles, mumps, rubella, chicken pox, yellow fever, influenza (intranasal vaccine) and oral polio vaccine. Attenuated life bacterial Vaccines include BCG and the oral typhoid vaccine.
Read more about immunization at immunosuppressed dermatology patients
Precautions while taking adalimumab
Infections
Because adalimumab works by selectively attacking TNF, theoretically it shouldn't have much of an effect on the rest of the body's immune system. However, caution should be exercised when considering its use in patients prone to infection or those with chronic or recurrent infections Concurrent Corticosteroid, azathioprine, or cyclosporine treatment increases the risk of infection. The infection may be due to bacteria, mycobacteria, invader mushrooms (disseminated or extrapulmonary histoplasmosis, aspergillosis, coccidioidomycosis) viral, parasitic or other opportunistic infectious agents.
There is particular concern that etanercept may reactivate tuberculosis (TB) (including the risk of Bacillus Calmette-Guérin [BCG]), viral hepatitis B, C, and increase the risk of infection by the human immunodeficiency virus (HIV). , listeria and legionella.
Vaccination with live vaccines (such as yellow fever, chicken pox, zoster, mumps / measles / rubella). [MMR], BCG) should be avoided.
Other risks
Adalimumab should also be used with caution in the following situations:
- Congestive heart failure - should not be used by patients with moderate or severe heart failure
- Pre-existing or recent start CNS demyelinating disorders (eg, multiple sclerosis)
- Skin patients Cancer or at high risk of skin cancer
- Patients with a history of cancer.
Patients receiving anakinra, a medicine used in rheumatoid arthritis, should not be prescribed adalimumab.
The safety of adalimumab during pregnancy and lactation is unknown. Therefore it is not recommended. Whenever possible, the drug should be discontinued several months before conception.
Patients requiring major surgery may be advised to temporarily discontinue adalimumab 2 to 3 months before a planned operation. It can be started again 2 weeks after surgery, provided there is no infection present.
Adalimumab side effects
Adalimumab appears to be well tolerated. Mild to moderate injection site reactions (redness, swelling, itching, pain) appear to be the most common side effect, occurring in 20% in patients. Mild to severe infections are the main risk of treatment and should be treated immediately.
Serious cutaneous reactions, including worsening psoriasis, have rarely been reported, vasculitis, anaphylaxis, Stevens-Johnson syndrome and toxic epidermal necrolysis
Like all medicines that work on the immune system, it can increase the risk of certain types of lymphoma (white blood cell cancer). They have rarely been reported in patients treated with adalimumab, generally in those who also take other medications that suppress the immune system, such as azathioprine or mercaptopurine.
Skin cancers, in particular scaly cell carcinoma, have also been reported in patients with adalimumab, generally in patients with other risk factors, such as sun-damaged skin or previous treatment with photochemotherapy (PUVA).
Monitoring while taking adalimumab
Regular follow-up visits are needed to monitor the safety and effectiveness of treatment. It is recommended that patients taking biologic medications undergo routine blood tests every 6 months or so, including a complete blood count and liver function tests. The TB test should also be repeated from time to time.
Adalimumab blood levels can be used to monitor adherence to therapy and determine the optimal dose in an individual.
Discontinue adalimumab
Adalimumab should be discontinued in the following circumstances:
- New serious infection (may be recommended when the infection has resolved)
- Unexplained severe systemic symptoms that may be due to infection
- Shortness of breath or other symptoms due to heart failure or chronic obstructive pulmonary disease
- Some elective surgical procedures: guidelines range from non-discontinuation of treatment up to one month before elective surgery. It can be restarted after the operation if there is no infection and wound healing is satisfactory.
- Cancer development, including lymphoma, solid cancer, Merkel cell carcinoma (an aggressive form of skin cancer associated with immunosuppression), or multiple squamous cell carcinomas. Basal Cell carcinoma generally does not lead to discontinuation of adalimumab.

