Ad
Skin cancer
Application to facilitate skin self-examination and early detection. read more.
What is a congenital melanocytic nevus?
A congenital melanocytic nevus (American spelling nevus) is a proliferation of benign melanocytes that are present at birth or develop shortly after birth [1]. This form of congenital nevus is also known as a brown birthmark.
Melanocytic similar naevior moles that were not present at birth, are often called “congenital melanocytic nevi such as nevi,” “congenital nevi,” or “late” nevi.
Naevi can also form from other skin cells (e.g. vascular nevi, which form from blood vessels) Some of these are also congenital (present at birth) and are described on other DermNet pages.
Classification of congenital melanocytic nevi
Congenital melanocytic nevi are generally classified by their size in an adult. There are several different classifications.
- A small congenital melanocytic nevus has <1,5 cm de diámetro.
- An average congenital melanocytic nevus measures 1.5–19.9 cm.
- A large or giant congenital melanocytic nevus is ≥ 20 cm in diameter.
A modification of the above criteria is used in some centers. [2] in an effort to increase classification accuracy.
- Small congenital melanocytic nevi have <1,5 cm de diámetro.
- Medium congenital melanocytic nevi are 1.5–10 cm.
- Large congenital melanocytic nevi measure between 11 and 20 cm.
- Giant congenital nevi are > 20 cm in diameter and are subdivided into:
- G1 (21–30 cm)
- G2 (31–40 cm)
- G3 (> 40cm).
2013 classification of congenital melanocytic nevi
In 2013, a new categorization of congenital melanocytic naevi was proposed using the predicted adult size [4]:
- Little (<1.5 cm)
- Medium (M1: 1.5–10 cm, M2: > 10–20 cm)
- Large (L1: > 20–30 cm, L2: > 30–40 cm)
- Giant (G1: > 40–60 cm, G2: > 60 cm)
- Satellite satellites: none, 1–20, > 20–50 and > 50 satellites.
Congenital melanocytic nevi should be described according to their body site, colors, surface characteristics, and whether or not there are hypertrichosis (hair)
Progression over time.
Congenital melanocytic nevi generally grow proportionally with the child. As a rough guide, the likely adult size of a congenital nevus can be calculated as follows:
- Lower limbs: adult size is x 3.3 at birth
- Upper limbs/torso: adult size is x 2.8 at birth
- Head: adult size is x 1.7 at birth.
Descriptive names of some congenital nevi.
Some congenital nevi are given specific descriptive names. Some of these are listed here.
Mottled lentiginous nevus
- Also called naevus spilus
- Dark spots on a flat tan background
- The number of spots may increase or decrease over time.
Satellite injuries
- It is located on the periphery of the central congenital melanocytic nevus or in any other part of the body.
- Smaller melanocytic nevi similar in appearance to
- Present in >70% of patients with a large congenital melanocytic nevus
late nevus
- Melanocytic naevi that appear after birth.
- Slower growth and less synthesis of melanin than congenital nevus [3]
- Histopathology is similar to true congenital melanocytic nevi
nevus garment
- The name refers to the anatomical location of nevus.
- Swimsuit nevus involves central areas usually covered by a swimsuit, for example, the buttocks
- Coat sleeve nevus involves an entire arm and proximal shoulder
Halo naevus
- Affects some congenital and late melanocytic nevi
- The surrounding skin becomes lighter or whiter
- The central injury may also become lighter and smaller and may disappear
- Due to immune destruction of melanocytes.
Congenital melanocytic nevi

Congenital nevus

Congenital nevus

Congenital nevus

Congenital nevus

Congenital nevus

Congenital nevus
How common are congenital melanocytic nevi?
- Small congenital nevi occur in 1 in 100 births [1, 2, 3]
- Medial congenital nevi occur in 1 in every 1000 births [3]
- Giant congenital melanocytic naevi are much rarer (1 in 20,000 live births) [1, 2, 3]
They occur in all races and ethnic groups, and men and women are equally at risk.
What are congenital melanocytic nevi like?
Congenital melanocytic nevi present in the form of one or several shades, round or oval pigmented patches [2]. They may have increased hair growth (hypertrichosis). The surface may be slightly rough or uneven.
Congenital nevi usually enlarge as the child grows, but can sometimes become smaller and less obvious over time. In rare cases, some may even disappear. However, they can also become darker, raised, more irregular and hairy, especially around the time of puberty.
Do congenital melanocytic nevi cause any symptoms?
Congenital melanocytic nevi are usually asymptomaticHowever, some can be itchy, particularly larger lesions. It is believed that there may be a reduced function of sebaceous (oil and eccrine (sweat glands), which can cause dry skin and an increased sensation of itching.
The overlying skin may become brittle and erode or ulcerate. Deep nests of melanocytes in the dermis can weaken the ties between epidermis and the dermis and represent the skin fragility [3].
Congenital melanocytic naevi are often unsightly, especially when they are extensive, that is, large or giant congenital melanocytic naevi. Therefore, they can lead to anxiety and deterioration of self-image, especially when the lesions are in visible areas.
Giant melanocytic nevi and, to a lesser extent, small lesions are associated with an increased risk of developing cutaneous melanoma, neurocutaneous melanoma and rarely other tumors (see below).
What causes a congenital melanocytic nevus?
Congenital melanocytic nevi are caused by located genetic abnormalities resulting in the proliferation of melanocytes; These are cells in the skin responsible for normal skin color. This abnormal proliferation is believed to occur between 5 and 24 weeks of gestation. If proliferation begins early in development, giant and medium-sized congenital melanocytic nevi form [1]. Smaller congenital melanocytic naevi form later in development after melanoblasts (immature melanocytes) have migrated from the neural crest to the skin [1].
In some cases, there is also an excessive growth of hair-forming cells and epidermis, forming an organoid nevus.
Very early onset of congenital nevus bBefore the separation of the upper and lower eyelids, the nevi are kissed, that is, one part of the nevus is on the upper eyelid and the other part is on the lower eyelid.
Naevi kisses
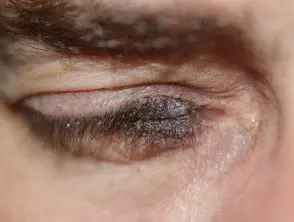
kissing naevus

kissing naevus
Molecular changes
The proto-oncogenes c-met and c-kit play important roles in melanocyte development. Hepatocyte growth factor, a cytokine (messenger protein) that regulates the proliferation and migration of melanocytes, may also be important in the development of congenital melanocytic nevi [1].
Neurocutaneous melanosis
Neurocutaneous melanocytosis is rare syndrome defined by the proliferation of melanocytes in the central nervous system (brain and spine cable) and the presence of a congenital melanocytic nevus [1,2]. Most cases are associated with a giant congenital melanocytic nevus and satellite lesions.
Neurocutaneous melanosis is estimated to affect 5–10% in people who have a giant congenital melanocytic nevus. However, most cases are likely to remain asymptomatic, and the true incidence remains unknown [3]. Melanocytes in the brain and spinal cord can often be detected by a Magnetic resonance scanning but the use of these scans is controversial because the condition is not easily treatable.
Neurocutaneous melanocytosis may present with symptoms of elevation intracranial pressure [2], such as:
- A headache
- Vomiting
- Irritability
- Focal cranial nerve signs
- Seizures
- Hydrocephalus
- Delayed development.
How is the diagnosis of congenital melanocytic nevus made?
The diagnosis of a congenital melanocytic nevus is usually based on clinical appearance. If there is any doubt, examine the lesion with dermatoscopy or take a sample from the lesion histology (biopsy) can show features microscopic features.
Dermoscopy
Evaluation of congenital melanocytic nevus by dermoscopy will reveal the pattern of pigmentation and its symmetry or lack of symmetry. The most common overall pattern of congenital or late melanocytic nevus is globular, but lattice, unstructured and mixed patterns can occur. The nevus may have different structures across the lesion, sometimes leading to an overall asymmetry of the structure.
Pathology
Congenital melanocytic nevi are usually larger than acquired nevi (which are melanocytic nevi that appear after 2 years of age), and the nevus cells often extend deeper into the dermis, fat layer, and structures. deeper. The cells of the nevus characteristically cluster around the blood vessels, the hair. follicles, sebaceous and eccrine glandsand other skin structures. Congenital nevus cells tend to affect collagen bundles in the deeper layers of the skin more than is the case in an acquired nevus [1,2].
Risk of developing melanoma within a congenital melanocytic nevus
The following features of congenital melanocytic nevus are associated with an increased risk of developing melanoma (a skin Cancer)
- Large or giant size
- Axial o paravertebral location (crossing the spine)
- Multiple congenital satellite naevi
- Neurocutaneous melanosis.
The risk of melanoma is mainly related to the size of the congenital melanocytic nevus. Small and medium-sized congenital melanocytic nevi have a very small risk, much lower than 1%. Melanoma is more likely to develop in giant congenital nevi (lifetime estimates are 5 to 10%), particularly in lesions that lie across the spine or where there are multiple satellite lesions. Melanoma can begin inside the nevus or within any neuromelanosis found in the brain and spinal cord. Very rarely, other tissues containing melanocytes can also be a source of melanoma, such as the gastrointestinal tract. mucous membrane. In 24% cases, the origin of the melanoma cannot be identified. [2].
Melanoma associated with a giant congenital melanocytic nevus or neuromelanosis can be very difficult to detect and treat.
The risk of developing melanoma is highest in early childhood; 70% melanomas associated with giant congenital melanocytic nevi are diagnosed at the age of ten years [1,3].
In rare cases, other types of tumor can develop within giant congenital melanocytic nevi including benign tumors (lipomas, schwannomas) and others evil one tumors (including sarcomas)
Melanoma can also develop within a small congenital melanocytic nevus. This is rare and is likely to occur in the periphery of the nevus during adult life.
Is regular monitoring recommended?
- It may be helpful to have a close-up photograph of the congenital nevus with a ruler next to it to evaluate size changes.
- Digital monitoring using dermoscopic imaging (mole mapping) may also be helpful in detecting changes in structure. However, such changes are normal in childhood and should not be a cause for concern.
- It is advisable to continue observation of neurodevelopment in those at risk for neurocutaneous melanosis [3].
Forecast of melanoma associated with congenital melanocytic nevus
Unfortunately, when a rare melanoma arises within a giant congenital melanocytic nevus, the prognosis is poor. This is due to the deeper origin of the tumor which makes it more difficult to detect on clinical examination, resulting in a later stage of presentation. The deeper location also facilitates early spread through blood and lymph vessels. In 24% cases, the melanoma has already spread to other sites (metastasis) at the time of first diagnosis.
Treatment of a congenital melanocytic nevus
Management of a congenital melanocytic nevus should take into account the subject's age, lesion size, location and depth, and the risk of developing malignant change within the lesion.
Giant congenital melanocytic nevus
The only definitive indication for surgery on a giant congenital melanocytic nevus is when melanoma develops inside it. [2].
Small congenital nevus
If a small congenital nevus is growing at the same rate as the child and is not otherwise changing, the usual practice is not to remove it until the child is old enough to cooperate with a local anesthetic injection, usually around 10 to 12 years old. Even then, removal is not essential.
Reasons to consider surgical removal may include:
- Unsightly appearance
- Difficulty observing the mole (eg, scalp, back)
- A recent change in the lesion (darkening, lumps, enlargement)
- Appearance similar to melanoma (irregular shape, variegated color).
Prophylactic surgical removal of a nevus
The following factors should be considered before prophylactic surgical removal of a nevus.
- Prophylactic excision of a small injury can be delayed until an age when the patient is old enough to make an informed decision [3].
- Small or medium-sized congenital melanocytic nevi have a low risk of developing malignant changes.
- Irregular, lumpy, or thick lesions or lesions that are difficult to evaluate clinically may have a lower threshold for considering surgical excision, so as not to miss a melanoma.
- The 50% melanomas diagnosed in those with giant congenital melanocytic naevi occur elsewhere in the body, such as within the central nervous system [2]. Therefore, surgical excision of the lesion may not eliminate the risk of melanoma.
- Large or giant melanocytic lesions may be too large to be completely removed.
- Large lesions may require a skin flap or graft to close the surgical defect.
Complications of surgery
Complications that can occur after surgery include:
- Flap graft or failure
- Infection
- Wound breakdown
- bleeding or hematoma
- Hypertrophic or keloid scar
- Irritable or itchy scar.
Other treatment options for a congenital melanocytic nevus
Dermabrasion
Dermabrasion may allow partial removal of a large congenital nevus; Deeper nevus cells may persist. Dermabrasion can lighten the color of the nevus but cannot reduce the growth of hair within it. May cause scarring.
Tangential excision (shaving)
Tangential or shave excision uses a blade to remove the top layers of skin (epidermis and upper dermis). This may reduce the pigmentation, but the lesion may not be completely removed. Excision by shaving can cause significant scarring.
Chemical peels
Chemical peels using trichloroacetic acid or phenol can lighten the pigmentation of a superficial (superficial) congenital nevus found in the upper layers of the skin.
To be ablation
Laser treatment is considered if surgical intervention is not possible. They can cause a lightening of the injury. Suitable devices include:
- Ruby Q-Switched To be
- Carbon dioxide coating laser
Techniques that result in partial removal of a congenital nevus may make the lesion more difficult to evaluate during long-term surveillance [2].


