What is dry skin?
Dry skin refers to skin that feels dry to the touch. Dry skin lacks moisture in the outer horny cell layer (stratum corneum) and this produces cracks in the surface of the skin.
Dry skin is also called xerosis, xeroderma or asteatosis (lack of fat).
Who dries their skin?
Dry skin can affect men and women of all ages. There is some racial variability in the water and lipid skin content.
- Dry skin that begins in early childhood can be one of about 20 types of ichthyosis (fish-scale skin). There is often a family history of dry skin.
- Dry skin is commonly seen in people with atopic dermatitis.
- Almost everyone over the age of 60 has dry skin.
Dry skin that starts later can be seen in people with certain diseases and conditions.
- Postmenopausal females
- Hypothyroidism
- Chronic renal disease
-
Malnutrition and weight loss.
- Subclinical dermatitis
- Treatment with certain medications such as oral. retinoids, diuretics and epidermal growth factor receiver inhibitors
People exposed to a dry environment may experience dry skin.
- Bass humidity- in desert climates or cool, windy conditions
- Excessive air conditioning
- Direct heat from a fire heater or fan.
- excessive bathing
- Contact with soaps, detergents and solvents.
- Inappropriate current agents such as alcohol
- Friction irritation from rough clothing or abrasives.
What causes dry skin?
Dry skin is due to abnormalities in the integrity of the barrier function of the stratum corneum, which is made up of corneocytes.
- There is an overall reduction in lipids in the stratum corneum.
- Ratio of ceramides, cholesterol and free fatty acids can be normal or altered.
- There may be a reduction in proliferation of keratinocytes.
- Keratinocytes The subtypes change in dry skin with a decrease in keratins K1, K10 and an increase in K5, K14.
- Involucrin (a protein) can be expressed early, increasing cell stiffness.
- The result is retention of corneocytes and a reduced water holding capacity.
Inherited forms of ichthyosis are due to loss of function. mutations in several genes (listed in parentheses below).
-
Ichthyosis vulgaris (FLG).
-
X-linked recessive ichthyosis (STS)
- Autosomal recessive congenital ichthyosis (ABCA12, TGM1, ALOXE3)
- Keratinopathic ichthyosis (KRT1, KRT10, KRT2)
Acquired ichthyosis may be due to:
- Metabolic factors: thyroid deficiency
- Illness: lymphomainternal malignancysarcoidosis HIV infection
- Drugs: nicotinic acid, kava, protein kinase inhibitors (eg, EGFR inhibitors), hydroxyurea.
What are the clinical features of dry skin?
Dry skin has a dull and rough surface, scaly quality. The skin is less flexible and cracked. When dryness is severe, the skin can become inflamed and cracked.
Although any site on the body can be dry, dry skin tends to affect pimples more than any other site.
The clinical features of ichthyosis depend on the specific type of ichthyosis.
Dry Skin

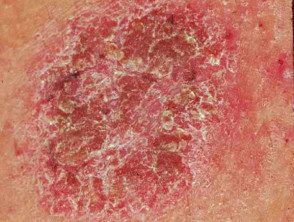
Ichthyosis

Ichthyosis close-up
Dry skin dermatitis.
See more images of dry skin.
dry skin complications
Dry areas of skin may be itchy, indicating a form of eczema/ dermatitis has developed.
-
Atopic eczema, especially in people with ichthyosis vulgaris
-
Eczema craquelé, especially in older people. Also called asteatotic eczema
- A dry form of nummular dermatitis /discoid eczema, especially in people who wash their skin excessively
When an older person's dry skin is itchy without a visible eruption, sometimes called winter itch, seventh age itch, senile pruritus or chronic itching of the elderly.
Other complications of dry skin can include:
-
skin infection when bacteria or viruses penetrate a break in the skin surface
- Overheating, especially in some forms of ichthyosis
-
Food allergy, for example, to peanuts, has been associated with filaggrin mutations
-
Contact allergy, for example to nickel, has also been correlated with barrier function defects.
How is dry skin type diagnosed?
Dry skin type is diagnosed by careful history and examination.
In children:
- Family history
- starting age
- Appearance at birth, if known
- Distribution dry skin
- Other features, eg, eczema, abnormal nail, hair, dentition, sight, hearing.
In adults:
- Medical history
- Medications and topical preparations.
- Frequency of bathing and use of soap.
- Evaluation of environmental factors that can contribute to dry skin.
sometimes a skin biopsy may be ordered Additional tests may be ordered to diagnose some types of ichthyosis.
What is the treatment for dry skin?
The basis of treatment for dry skin and ichthyosis are moisturizers /emollients. They should be applied liberally and often enough to:
- reduce itching
- Improves barrier function
- prevent the entry of irritantsbacteria
- Reduce transepidermal loss of water
When considering what emollient is the most suitable, consider:
- severity of dryness
- Tolerance
- personal preference
- Cost and availability.
Emollients generally work best if applied to damp skin, if pH is below 7 (acidic), and if it contains moisturizers such as urea or propylene glycol.
Additional treatments include:
-
Topical steroids if itching or dermatitis: choose an emollient base
- Topical calcineurin inhibitors if topical steroids are not suitable.
How can dry skin be prevented?
Eliminate aggravating factors.
- Reduce the frequency of bathing.
- A humidifier in winter and air conditioning in summer.
- Compare having a short shower with a long bath.
- Use warm water, not hot.
- Replace standard soap with a substitute such as a synthetic detergent cleanser, water-miscible emollient, bath oil, antibacterialpruritus tar oil, colloidal oatmeal, etc.
- Apply an emollient liberally and often, especially soon after bathing and when itchy. The drier the skin, the thicker it should be, especially on the hands.
What is the prognosis for dry skin?
The tendency to dry skin may persist throughout life, or may improve once contributing factors are controlled.

