Introduction
Skin, hair and the nail tissue is collected to microscopy and culture (mycology) tor establish or confirm the diagnosis of a fungus infection.
Exposing the site to long wavelengths Ultraviolet radiation (Wooden lamp) can help identify some fungal hair infections (tinea capitis) because infected hair is fluorescent green.
Collection of samples for fungal tests.
Samples for microscopy and fungal culture. They are transported to the laboratory in a sterile container or in a black paper envelope. They include:
- Scrapping of scale, best taken from the forefront of the eruption after cleaning the skin with alcohol
- Skin stripped with masking tape, which is then affixed to a glass slide
- Hair that has been pulled from the roots.
- Brushed from an area climbing on the scalp
- Nail clippings or scraped skin under a nail
- A skin biopsy
- A wet swab of a mucous membrane surface (inside the mouth or vagina) in a special means of transport.
You should also take a cotton swab pustules in case of secondary bacterial infection.
Direct microscopy of skin scrapings and nail clippings.
The material is examined by microscopy using one or more of these methods:
- Preparation of potassium hydroxide (KOH), stained with blue or black ink
- Fluorescent staining
- A wet mount without smudges
- A stained dry spot
- Histopathology biopsy with special stains, such as periodic Schiff's acid (PAS).
Microscopy can identify a dermatophyte by the presence of:
- Fungal hyphae (branched filaments) that form a mycelium
- Arthrospores (broken spores)
- Arthroconidia (specialized external spores)
- Spores inside a hair (endothrix) or outside a hair (ectothrix).
Fungal elements are sometimes difficult to find, especially if the tissue is highly inflamed, so a negative result does not rule out yeast infection.
A yeast infection can be identified by the presence of:
- Yeast cells, which can divide by budding
- Pseudohyphae (branched, dermatophyte-like filaments) that form a pseudomycece.
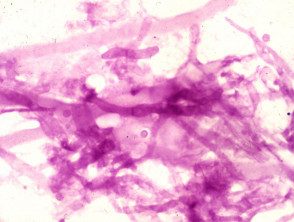
PAS stain from Aspergillus seen on a skin biopsy

KOH by M. canis

Candida KOH
Mushroom cultivation
Culture identifies what organism is responsible for the infection:
- To find out the source of infection, eg. a particular animal
- To select the most suitable treatment.
Cultivation of the fungus in culture can take several weeks, incubated at 25–30 ° C. The specimen is inoculated in a medium such as Sabouraud's dextrose agar containing cycloheximide and chloramphenicol. Cycloheximide is left out if a template requires identification.
A negative culture may arise because:
- The condition is not due to a fungal infection.
- The specimen was not collected correctly.
- Antifungal treatment had been used prior to sample collection.
- There was a delay before the sample reached the laboratory.
- Laboratory procedures were incorrect.
- The organism grows very slowly.
Yeast and mold culture may be due to harmless colonization rather than infection; This is common in an underlying skin condition like psoriasis.
Cultural slopes

Non-inoculated leather scraping earrings. The blue top is Sabouraud dextrose agar with antibiotics and the white top is a dermatophyte test medium.

Morphology of the Trichophyton rubrum colony on potato dextrose agar culture plates showing reddish pigmentation at the back of the slope.

Rhodotorula grown on Sabouraud dextrose agar with antibiotics
Blood tests for patients with disseminated fungal infection
Blood tests are not helpful in diagnosing superficial fungal infections. In subcutaneous and systemic Mycosis, various tests may be helpful.
- Culture
- Antibodies (histoplasmosis, coccidioidomycosis)
- Antigen (cryptococcosis, aspergillosis, candidiasis, histoplasmosis).
Molecular biology techniques
Point-of-care tests for some yeast infections are reported to be accurate, but not yet widely available.

