What is it urticaria?
Urticaria is a condition characterized by the presence of cure (urticaria) or angioedema (swelling of the skin) [1,2].
- A bump is a red or pale superficial swelling on the skin that is often surrounded by erythema. A cure can persist from a few minutes to 24 hours.
- Angioedema is a deeper skin-colored or red swelling within the skin or mucous membranes May take up to 72 hours to resolve.
Hives affect up to one in four people at some point in their lives and are classified by duration, acute or chronicand cause, whether spontaneous or inducible [1–3].
Acute urticaria is the daily or episodic appearance of scarring, angioedema, or both for less than 6 weeks. [1,2]. Causes may include infections and allergies, but more often, the cause is unknown [2].
Figure 1. Classification of urticaria.
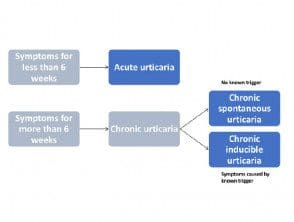
Classification of urticaria
Types of hives

Spontaneous urticaria

Angioedema

Dermographism
What is chronic urticaria?
Chronic urticaria is the daily or episodic appearance of scarring, angioedema, or both for 6 weeks or longer. [1,2]. Chronic hives may persist for a duration ranging from a few months to many years. [2,4].
International guidelines for the classification, diagnosis and management of chronic urticaria have recently been published, based on a consensus of multiple national and international societies. [1].
Chronic urticaria is spontaneous or inducible; both types can coexist in a patient [1,2]. (See DermNet NZ page on chronic spontaneous urticaria.)
What is chronic inducible urticaria?
Chronic inducible urticaria is chronic urticaria that has an attributable cause or trigger and is classified according to the stimulus that causes scar development. Commonly, these stimuli that cause scar development include stroking or scratching the skin (dermographism), exercise, and emotional distress (cholinergic urticaria).
Less common forms of chronic inducible urticaria are triggered by cold, heat, pressure, sunlight (solar urticaria), contact with water or various chemicals (contact urticaria), or vibration. [1,2].
Who gets chronic inducible urticaria?
Chronic urticaria is reported to affect 1.8% of the population [2]. the predominance of inducible chronic urticaria is approximately 0.5% (15-25% of all cases of chronic urticaria) [3].
Women experience hives and chronic hives almost twice as often as men [2,4]. Although urticaria in children is common, they are more likely to present with spontaneous chronic urticaria than with inducible chronic urticaria [2].
What are the clinical characteristics of chronic inducible urticaria?
Chronic inducible urticaria usually presents with scarring [1,2]. Scars can appear anywhere on the body. [2,5].
- Scars vary in size from a few millimeters to several centimeters.
- They are white or red in color and are often surrounded by a red flare.
- In chronic inducible urticaria, scars usually appear about 5 minutes after stimulation and last from a few minutes to 2 hours. [5].
- The marks can change shape before resolving: they can be round and form rings or a map-like pattern.
Characteristically, the riches are:
- Linear in symptomatic dermographism
- Confined to contact areas in contact urticaria
- Diffuse in cold urticaria (if large areas of skin are affected, angioedema can also occur in cold urticaria).
Angioedema can rarely be induced within minutes of exposure to a vibratory stimulus. [5]. Delayed pressure can cause hives and angioedema.
Symptoms are usually limited to areas of skin that are exposed to a specific trigger. Individual patients may present with two or more subtypes of chronic inducible urticaria. [6].
Inducible urticaria

Linear riches in dermographism

Round and linear riches in dermographism

Dissemination of the ice cube test in cold urticaria
What causes chronic inducible urticaria?
Hives are a mast cells-measure of illness. Activated mast cells launching histamine together with other mediators, such as plateletactivation factor and cytokines, resulting in the activation of the sensory nerve, vasodilation, plasma extravasationand recruitment of cells to urticarial injury. Mast cells can be activated by many different molecules in urticaria, but in general, these are not well defined [1].
Scarring and angioedema are induced by environmental or physical stimuli in inducible chronic urticaria. [1,2]. The different types of inducible urticaria and their triggers include:
-
Dermographism: caused by scratches or tight clothing
-
Cold hives: caused by cold air, cold water, ice or cryotherapy
-
Cholinergic urticaria: as a result of increased body heat due to exercise, emotional discomfort, or a hot shower
-
Contact urticaria: where a trigger substance is absorbed through the skin or a mucous membrane; this can be a allergen like latex or semen (immunoglobulin mi [IgE] mediated), a pseudoallergen or a irritating (like a medicine, a nettle, or a hairy caterpillar)
-
Delayed pressure hives: as a result of pressure on the affected area several hours before, such as from a heavy bag, seat belt, or sitting on a horse
-
Solar urticaria: due to exposure to sunlight, mainly affecting skin that is infrequently exposed to the sun
-
Heat hives: caused by a hot water bottle or hot drink
-
Urticaria or aquagenic angioedema – caused by water
- Vibratory angioedema: A result of vibratory activities such as using a jackhammer, mowing the lawn, or riding a motorcycle.
What are the complications of chronic urticaria?
The burden of chronic urticaria is substantial for patients, their families and caregivers, the health system, and society. [1,3]. Chronic hives can cause sleep deprivation, anxiety, depression, lack of energy, and social isolation. [7] and lead to a significant deterioration in quality of life [1,3].
How is chronic inducible urticaria diagnosed?
Chronic inducible urticaria is diagnosed by taking a careful history and examination; This diagnosis is based on a history of daily or episodic healing for more than 6 weeks that has been induced by an external stimulus.
International guidelines provide a diagnostic algorithm for chronic urticaria (see figure 2). The diagnosis of chronic inducible urticaria is based on provocative testing and then compiling a complete history that covers:
- When the hives started
- The shape, size, frequency and distribution of the riches
- The presence of angioedema.
- The presence of pain in the bones or joints, feveror abdominal pain
- Previous or family history of diseases and angioedema.
- If the diseases were induced by physical agents or exercise
- If the presence of corresponds to a time of day, work, recreation, menstrual cycle, vacation or trips abroad
- The effect of food or drugs on hives (eg, nonsteroidal anti-steroids).inflammatory drugs [[NSAID]and angiotensin conversion enzyme [ACE] inhibitors)
- Any association with infections or psychosocial stress
- Any history of allergies or systemic disease
- Occupational history, hobbies and activities.
- Previous treatment and response
- Diagnostic procedures and results. [1].
Figure 2. Diagnostic algorithm for chronic urticaria.
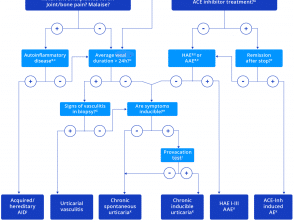
Diagnostic algorithm for chronic urticaria.
Credit: Zuberbier et al. Allergy 2018.
Notes on the diagnostic algorithm for chronic urticaria
- In addition to ACE inhibitors, other renin inhibitors and sartans have also been reported to induce angioedema, but much less frequently.
- Patients should be asked for a detailed family history and age at onset of illness.
- Test for elevated inflammatory markers (e.g., CRP and ESR), test for paraproteinemia in adults, look for signs of neutrophil-rich infiltrates in skin biopsies, and perform genetic mutation analysis for hereditary periodic fever syndromes (e.g. ., Periodic syndromes associated with cryopyrin) if highly suspected
- Patients should be asked: “How long does each cure last?”
- Test C4 complement and C1 inhibitor levels and function; also test C1q and C1 inhibitory antibodies if angioedema is acquired and suspected; and do genetic mutation analysis if previous tests are unremarkable but the patient's history suggests hereditary angioedema.
- If there is no remission after 6 months of ACE inhibitor discontinuation, test C1 inhibitor levels.
- Does biopsy of lesional skin show damage to small vessels in the papillary and reticular dermis and fibrinoid deposits in perivascular and interstitial locations suggestive of urticarial vasculitis?
- Patients should be asked: “Can you make your scars appear? Can you bring out your riches?
- In patients with a history suggestive of inducible urticaria, standardized provocation tests should be performed according to the international consensus recommendation. [16].
- Acquired autoinflammatory syndromes include Schnitzler syndrome, systemic juvenile idiopathic arthritis, and adult-onset Stills disease; Hereditary autoinflammatory syndrome includes cryopyrin-associated periodic syndromes, such as familial cold autoinflammatory syndrome, Muckle-Wells syndrome, and neonatal-onset multisystem inflammatory disease, more rarely hyper-IgD syndrome and factor receptor-associated periodic syndrome. of tumor necrosis.
- In some rare cases, recurrent angioedema is neither mast cell-mediated nor bradykinin-mediated, and the underlying pathomechanisms remain unknown. Some cases call these rare cases “idiopathic angioedema.”
Consensus recommendations for diagnostic testing and treatment of chronic inducible urticaria can be used to identify the subtype of chronic inducible urticaria and to assess disease activity. [1,6].
Provocation testing is used to determine relevant triggers and to assess activation thresholds. Provocation testing in positive patients usually results in the development of urticaria within a few minutes. An exception is delayed pressure urticaria, where it may be necessary to wait several hours for a response. [6].
In patients with negative provocation responses, where chronic inducible urticaria is strongly suspected from the patient's history, the test should be repeated. Ideally, testing should be performed on a previously affected skin site, although testing should not be performed if scarring has occurred at this site in the previous 3 days [6].
Challenge test results may be affected by medication; therefore, symptomatic treatment should be discontinued before testing, if possible. Antihistamines should be stopped 3 days before the test and should be systematic. glucocorticoids 7 days before the test [6].
A sample form for documenting challenge testing is shown in Figure 3. [6].
Figure 3. Provocation tests for chronic inducible urticaria.
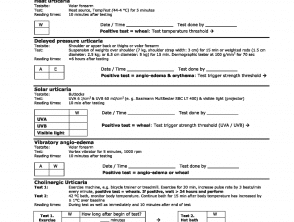
Provocation tests for inducible urticaria.
Credit: Magerl M, et al. Allergy 2016.
Which is the differential diagnosis for chronic inducible urticaria?
The differential diagnosis depends on the specific type of chronic inducible urticaria and includes other forms of inducible and spontaneous urticaria, which may coexist [8].
-
Dermographism and delayed pressure urticaria may present with a similar history.
-
Cholinergic urticaria can be confused with exercise-induced urticaria. anaphylaxis.
-
Aquagenic urticaria can be confused with aquagenic pruritus, cholinergic urticaria, cold urticaria and local heat urticaria.
-
Solar urticaria can be confused with sunburn or another form of photosensitivity, as:
- Polymorphous light eruption
- Erythropoietic protoporphyria
- Drug-induced photosensitivity
- Cutaneous lupus erythematosus.
Assessment of disease activity and control
In addition to diagnosis, activation threshold measurements are also used during treatment to measure disease activity and response to ongoing treatment [1,6].
The urticaria control test (UCT) [9] is useful in evaluating the disease status of patients and is validated to determine the level of disease control in both spontaneous chronic urticaria and inducible chronic urticaria. [1]. The UCT has only four items with a clear cutoff for “well-controlled” versus “poorly controlled” disease, making it useful in routine clinical practice.
The Angioedema Activity Score (AAS) allows the patient to rate each of the five key factors related to their symptoms from 0 to 3 (giving a daily score of 0 to 15) [10]. The daily AAS can be summed to provide 7-day (AAS7), 4-week (AAS28), and 12-week (AAS84) scores [10].
Quality of life
Validated instruments can be used to assess the emotional impact of chronic urticaria and the effect on patient quality of life, such as the Chronic Urticaria Quality of Life Questionnaire (CU-Q).2oL) [11] and the Angioedema Quality of Life Questionnaire (AE-QoL) [1,12].
What is the treatment for chronic inducible urticaria?
Treatment aims to control symptoms [1,2].
The approach to treating chronic inducible urticaria may involve:
- Avoid triggers
- Tolerance induction
- Pharmacological treatment to prevent the release of mast cell mediators or to prevent the effects of mast cell mediators [1].
Avoid triggers
It is often difficult for patients with chronic inducible urticaria to completely avoid the physical stimuli that trigger healing. [1]. It is recommended that patients minimize exposure to triggers as much as possible, although tolerance induction (described below) requires daily exposure to a trigger.
Inducing tolerance
Inducing tolerance may be useful in cold urticaria, cholinergic urticaria, and solar urticaria. Tolerance induction lasts only a few days, and consistent daily exposure is required to maintain tolerance [1].
Pharmacological treatment of chronic urticaria.
An algorithm for treating chronic urticaria is included in international guidelines (see figure 4) [1], these guidelines should be used with caution in children and pregnant/nursing women. Drugs that are contraindicated in pregnancy it should not be used [1].
Treatment should be continued as needed until the hives have disappeared.
Figure 4. Pharmacological treatment algorithm.
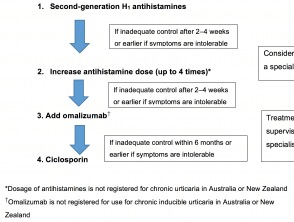
Pharmacological treatment algorithm for chronic urticaria.
Credit: Zuberbier et al, Allergy 2018.
Antihistamines
Some forms of chronic inducible urticaria are mediated by histamine. Intermittent or continuous treatment with H1-antihistamines is supported by clinical trial data [1,2].
Non-sedating antihistamines are preferred to older antihistamines, which have anticholinergic effects and sedative actions. [1]. First-line symptomatic treatment for chronic inducible urticaria includes:
- Cetirizine
- Ebastina
- Loratadine
- Fexofenadine
- Desloratadine
- Levocetirizine
- Rupatadine
- Bilastine
Terfenadine and astemizole are no longer available in New Zealand or Australia because they are cardiotoxic in combination with ketoconazole or erythromycin. [1].
If standard doses are not effective, doses of bilastine, loratadine, cetirizine, desloratadine, ebastine, fexofenadine, levocetirizine, and rupatadine can be increased up to four-fold (note that some of these agents are not available and higher doses are not are licensed) in New Zealand or Australia) [1].
Most patients with chronic inducible urticaria who do not respond to standard doses of antihistamines will benefit from ascending dosing, but antihistamines are not always effective. [1]. Located Heat urticaria, aquagenic urticaria, and vibratory urticaria rarely respond to antihistamines.
Treatment of refractory inducible chronic urticaria
About one-third of patients continue to have symptoms despite maximum tolerated daily doses of antihistamine. [3]. Patients with refractory inducible chronic urticaria should be referred to a dermatologist, immunologist or medical allergy specialist [1].
Omalizumab
Omalizumab has been reported to be effective in chronic inducible urticaria [1], including cholinergic urticaria [13], cold urticaria [14,15], solar urticaria [16], heat urticaria [17], symptomatic dermographism [18,19]. and delayed pressure urticaria [20].
Note: Omalizumab is not indicated for the treatment of patients with chronic inducible urticaria in New Zealand or Australia.
Cyclosporine
No published trials have specifically investigated the use of cyclosporine in patients with chronic inducible urticaria, although one case series (n = 100) investigating its use in the treatment of chronic spontaneous urticaria included patients who also had chronic inducible urticaria (45% of cases ) Control was achieved with cyclosporine or omalizumab in some cases refractory to antihistamines. [twenty-one].
Note: Ciclosporin is not indicated for the treatment of patients with chronic inducible urticaria in New Zealand or Australia.
Corticosteroids
-
Systemic corticosteroids have not been studied in randomized controlled trials, and evidence for their use in chronic inducible urticaria is limited. [1,2].
- Long-term use of systemic corticosteroids should be avoided as high doses are often required to reduce the symptoms of urticaria with the associated potentially serious adverse effects. [1,2].
- Se puede considerar un curso corto de corticosteroides en casos de graves exacerbations de urticaria crónica inducible, pero esto no siempre es efectivo [1,2].
Phototherapy
La fototerapia ha tenido éxito en el tratamiento de pacientes con urticaria crónica inducible, particularmente en pacientes con dermografismo. [1]. La forma más común de fototerapia utilizada es la fototerapia ultravioleta B de banda estrecha. [8].
Other treatments
Hay poca evidencia para apoyar cualquier otro tratamiento para la urticaria crónica inducible.
Immunomodulator los tratamientos pueden ser valiosos para pacientes individuales en situaciones clínicas particulares (p. ej., dapsona para la urticaria por frío) [8].
What is the outcome of chronic inducible urticaria?
La urticaria crónica inducible puede resolverse con el tratamiento de los síntomas y evitando los estímulos físicos que desencadenan la urticaria. Sin embargo, en muchos pacientes, el umbral para el desencadenante físico relevante es bajo y es casi imposible evitar los síntomas por completo. [1].
