What is it actinic keratosis?
Actinic keratosis is a scaly spot found on sun damaged skin. It is also known as solar keratosis. Is considered precancerous or an early form of cutaneous scaly cell carcinoma (a keratinocytes Cancer)
who gets actinic keratosis?
Actinic keratoses affect people who have often lived in the tropics or subtropics and have predisposing factors such as:
- other signs of photoaging skin
- Fair skin with a history of sunburn.
- History of long hours outdoors for work or recreation.
- faulty immune system
What causes actinic keratoses?
Actinic keratoses are a reflection of abnormal skin cell development due to DNA shortwave UVB damage.
They are more likely to appear if immune function is impaired, due to aging, recent sun exposure, predisposing disease, or certain medications.
What are the clinical features of actinic keratosis?
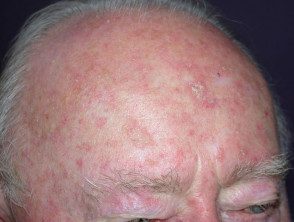
Actinic keratoses may be solitary, but there are often multiple keratoses. Appearance varies.
- A flat or thickened papule or license plate
- White or yellow; scaly, warty or horny surface
- Skin color, red or pigmented
- tender or asymptomatic
Actinic keratoses are very common on sites repeatedly exposed to the sun, especially on the back of the hands and face, and most commonly affect the ears, nose, cheeks, upper lip, lower lip vermilion, temples, forehead and bald scalp. In severely chronically sun-damaged individuals, they can also be found on the upper trunk, upper and lower extremities, and the backs of the feet.
Actinic keratoses

Actinic keratoses

Actinic keratoses

Actinic keratoses

Actinic keratoses

Actinic keratoses
Actinic keratoses
Many more images of actinic keratoses…
- Keratosis on the nose
- Keratoses on the face
- Keratosis on the scalp
- Keratoses on the hands
- Keratoses on the legs
- Keratoses treated with imiquimod
Complications of actinic keratoses.
The main concern is that actinic keratoses predispose to squamous cell carcinoma. It is rare for a solitary actinic keratosis to progress to squamous cell carcinoma (SCC), but the risk of SCC occurring at any time in a patient with more than 10 actinic keratoses is thought to be approximately 10 in 15%. A tender, thickened, ulcerated, or enlarged actinic keratosis is suspicious for SCC.
Cutaneous horn it can arise from an underlying actinic keratosis or SCC.
Because they are damaged by the sun, people with actinic keratoses are also at risk of developing actinic cheilitis, basal cell carcinoma (BCC, which is more common than SCC), melanoma and rare forms of skin cancer such as Merkel cell carcinoma.
How is actinic keratosis diagnosed?
Actinic keratosis is generally easy to diagnose clinically or by dermoscopy (see actinic keratosis dermoscopy). Occasionally a biopsy it is necessary, for example, to exclude SCC, or if treatment fails.
What is the treatment for actinic keratoses?
Actinic keratoses are usually removed because they are unsightly or uncomfortable, or because of the risk of skin cancer developing on them.
Treatment of an actinic keratosis requires the removal of defective skin cells. Epidermis regenerates from the environment or follicular keratinocytes who have escaped sun damage.
Soft, thickened, ulcerated, or dilated actinic keratoses should be treated aggressively. Asymptomatic keratoses planas may not require active treatment, but should be kept under observation.
physical treatments
Physical treatments are used to destroy individual keratoses that are usually symptomatic or have a thick, hard surface. scale. The lesions may reappear in time, in which case they can be treated again with the same or another method.
Cryotherapy using liquid nitrogen
Liquid nitrogen spray it is necessary to ensure adequate depth and duration of freezing. This varies according to injury location, width and thickness. Healing ranges from 5-10 days on the face, 3-4 weeks on the hands, and 6 weeks or more on the legs. Mild freezing for a superficial actinic keratosis usually leaves no mark, but longer freezing times result in hypopigmentation or scar.
Shaving, curettage and electrocautery
Shaving, curettage (scraping with a sharp instrument), and electrocautery (burning) may be necessary to remove a cutaneous horn or hypertrophic actinic keratosis. Wound healing takes several weeks or longer, depending on the body site. A specimen is sent to pathological examination.
Excision
Excision ensures that the actinic keratosis has been completely removed, which should be confirmed by pathology. The surgical wound is sutured (stitched). The sutures are removed after a few days, the time depending on the size and location of the lesion. The procedure leaves a permanent scar.
field treatments
The creams are used to treat areas of sun damage and AKs, sometimes after physical treatments have been done. Field treatments are most effective on facial skin. Pretreatment with keratolytics (such as urea cream, salicylic acid ointment or current retinoid), and thorough cleansing of the skin improves response rates. Results are variable and the course of treatment may need to be repeated from time to time. With the exception of diclofenac. gel, field treatments result in local inflammatory reactions such as redness, blistering and discomfort for a variable period of time.
-
Diclofenac is most often used as anti-inflammatory drug. Applied as a gel twice daily for 3 months, it is fairly well tolerated in the treatment of actinic keratoses, but less effective than the other options listed here.
-
5-fluorouracil is a cytotoxic agent. The cream formulation is applied once or twice daily for 2 to 8 weeks. 5-fluorouracil cream is sometimes combined with salicylic acid. Its effect can be enhanced with calcipotriol ointment.
-
Imiquimod cream is an immune response modifier. It is applied 2 or 3 times a week for 4 to 16 weeks.
- Photodynamic PDT therapy involves the application of a photosensitizer (a porphyrin chemicals such as methyl aminolevulinic acid) on the affected area before exposing it to a visible light source.
-
Ingenol mebutate gel is effective after only 2–3 applications.
Prevention of actinic keratoses.
Actinic keratoses are prevented by strict sun protection. If already present, keratoses can improve with a broad-spectrum sunscreen with a very high sun protection factor (50+) applied at least daily to affected areas, year-round.
The number and severity of actinic keratoses can also be reduced by taking 500 mg of nicotinamide (vitamin B3) twice a day.
What is the prognosis for actinic keratoses?
Actinic keratoses can recur months or years after treatment. The same treatment or another method used can be repeated. Patients who have been treated for actinic keratoses are at risk of developing new keratoses. They are also at higher risk of other types of skin cancer, especially intraepidermal squamous Cell Carcinoma, invader cutaneous squamous cell carcinoma, basal cell carcinoma and melanoma.

