What is aspergillosis?
Aspergillosis is a disease caused by aspergillus.
What is aspergillus?
Aspergillus is a fungus (mold) found in abundance throughout the environment in soil, decomposing plant matter, ornamental plants, water, house dust and building materials. More than 100 different species of aspergillus have been identified, but the species most commonly implicated in human disease are A. fumigatus, A. flavusand A. niger.
Who gets aspergillosis?
Aspergillosis is most often diagnosed when conditions that result in impaired immunity become more predominant. For example, invader Aspergillosis is estimated to occur in 5 to 13% of bone marrow transplant recipients, in 5 to 25% of patients who have received heart or lung transplants, and in 10 to 20% of patients receiving intensive treatment. chemotherapy for leukemia.
The term aspergillosis is not used to refer to chronic Nail infections caused by aspergillus, which is a form of onychomycosis that affects people with normal immune systems.
How does aspergillosis occur?
Aspergillus most commonly enters the human body through inhalation. Most people breathe in Aspergillus spores every day, with no ill effects. However, in patients with pre-existing medical conditions, aspergillus can begin to proliferate and cause disease, primarily a lung. infection. Infection is more likely if a large number of spores are inhaled, such as when exposed to a very dusty environment or during building renovation.
In rare cases, the fungus can enter through the skin (primary cutaneous aspergillosis), particularly in patients with thermal burns or trauma. Occasionally, outbreaks of primary cutaneous aspergillosis are due to contaminated biomedical equipment.
Aspergillus can also spread to the skin through the bloodstream.
What are the clinical characteristics of aspergillosis?
There are four common clinical patterns of disease.
Acute invasive aspergillosis
- Acute invasive apsergillus has a rapid onset and the disease progresses rapidly.
- The fungus invades and damages body tissues; most commonly the lungs and/or sinuses, but can spread throughout the body through the bloodstream.
- Symptoms include fever, cough, shortness of breath, chest pain, facial swelling, nosebleed, bulging of one eye, or neurological symptoms Other symptoms develop if the infection spreads beyond the lungs and sinuses.
- There is a high mortality rate.
Acute invasive apsergillus affects people with severely impaired immunity, particularly those:
- who has had bone marrow transplant or solid organ transplant
- on high doses of corticosteroids or chemotherapy for cancers such as leukemia
- with advanced HIV infection.
allergic aspergillosis
- Allergic aspergillosis is a allergic reaction to the aspergillus fungus in the lungs and/or paranasal sinuses.
- Pulmonary symptoms include fever, wheezing and cough. Patients may cough up blood or mucous plugs
- Breast Symptoms include facial pressure, headache, stuffy nose, yellow or green download of the nose and cough.
Allergic aspergillosis can affect anyone, but it is more common in people with asthma or cystic fibrosis.
Aspergilloma
- Aspergilloma is a “mushroom ball” that develops in a preexisting lung cavity.
- It may cause no symptoms or the patient may cough up blood (which can be profuse and life-threatening).
- Aspergillomas can also develop in other organs.
Aspergilloma affects people with an underlying lung disease that causes cavities, such as tuberculosis, emphysema, or cystic fibrosis.
Chronic necrotizing pulmonary aspergillosis
- Chronic necrotizing pulmonary aspergillosis is a rare condition that causes the death of tissue within the lungs.
- This form of aspergillosis progresses slowly over weeks or months.
- Symptoms often include fever, cough, night sweats, and weight loss.
- Chronic necrotizing pulmonary aspergillosis usually affects people with mild immune impairment, such as underlying lung disease, alcoholism, or who are on long-term corticosteroid treatment.
What are the skin manifestations of aspergillosis?
Skin changes are most commonly a consequence of extended Aspergillus infection in patients with impaired immunity.
- About 5 to 10% of patients with invasive aspergillosis develop skin lesions.
- Lesions include single or multiple red or violet indurations plates or papules. The lesions may be tender or symptom-free. As the lesions evolve, pus- or blood-filled blisters develop in the center, which eventually become necrotic blackened ulcers or scabs. Lesions most commonly appear on the extremities and head, and can affect a small or large area.
Primary cutaneous aspergillosis most often develops at the site of insertion of an intravenous cannula or venipuncture (blood test wound).
- Occlusive Dressings may increase the risk of developing primary cutaneous aspergillosis.
- Located Immunosuppression due to intralesional steroid injection may be associated with cutaneous aspergillosis.
- The lesions initially appear similar to cellulitis, then become necrotic ulcer or scab
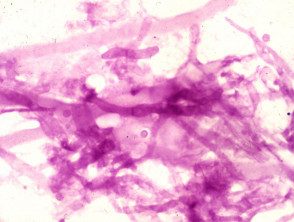
Cutaneous aspergillosis

Aspergillus skin lesion

Cutaneous aspergillosis

Cutaneous aspergillosis
How is aspergillosis diagnosed?
- Samples of sputum, blood or affected tissue can be grown in the laboratory to grow aspergillus.
- The fungus may be visible under a microscope in biopsies of affected tissue. Special mushroom stains may be necessary, but other mushrooms may look almost identical.
- chest x-ray or Connecticut Examination of the lungs may reveal characteristic abnormalities.
- A newer one antigenA test based on detecting evidence of invasive aspergillosis in the blood is available. However, the accuracy of this test appears to be variable.
Aspergillus in the laboratory.
Potassium hydroxide culture
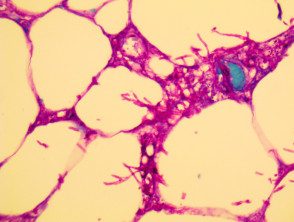
Histopathology
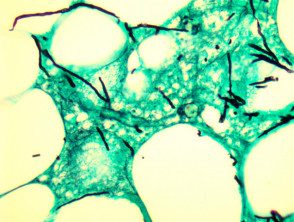
Histopathology
How is aspergillosis treated?
-
Voriconazole is currently used as a first-line treatment for invasive aspergillosis.
- Other medications used to treat aspergillosis include itraconazole, amphotericin B, caspofungin, micafungin, and posaconazole.
- Long-term treatment is usually required.
- When possible, immunosuppressive therapy, such as systemic corticosteroids, should be discontinued.
- Surgical removal of the infected lung cavity may be necessary in the case of aspergilloma.
Can aspergillosis be prevented?
Because the Aspergillus fungus is present everywhere in the environment, it is virtually impossible to avoid it completely. In patients with severely impaired immunity, the following measures may be useful:
- Avoid dusty environments, construction sites, gardening and grass cutting.
- Wear protective masks when near dusty environments
- Take preventative antifungal medications if recommended by your doctor.
- Use a high-efficiency particulate air (HEPA) filter in the hospital to prevent hospital-acquired lung infection in patients with low immunity.

