Ad
Skin cancer
Application to facilitate skin self-examination and early detection. read more.
What is it basal cell carcinoma?
Basal cell carcinoma (BCC) is a common local disorder. invader, keratinocytes Cancer (also known as non-melanoma cancer). It is the most common form of skin cancer. BCC is also known as rodent ulcer and basaloma. Patients with BCC often develop multiple primary tumors over time.
Who gets basal cell carcinoma?
Risk factors for BCC include:
- age and sex: BCCs are particularly predominant in older men. However, they also affect women and younger adults.
- Previous BCC or other form of skin cancer (scaly cell carcinoma melanoma)
- Sun damage (photoaging, actinic keratosis)
- Repeated past episodes of sunburn
- Light skin, blue and blonde or red eyes. hair-Note; BCC can also affect darker skin types.
- Previous cutaneous injury, thermal burn, disease (for example, cutaneous lupus, sebaceous nevus)
- Hereditary syndromes: BCC is a particular problem for families with basal cell naevus. syndrome (Gorlin syndrome), Bazex-Dupré-Christol syndrome, Rombo syndrome, Oley syndrome and xeroderma pigmentosum
- Other risk factors include ionizing radiation, exposure to arsenic, and immunosuppression due to illness or medications
What causes basal cell carcinoma?
The cause of BCC is multifactorial.
- Very often, there are DNA mutations in patching (PTCH) tumor suppressor gene, part of the hedgehog signaling pathway
- These can be caused by exposure to Ultraviolet radiation
- Various spontaneous and hereditary genetic defects predispose to BCC
What are the clinical characteristics of basal cell carcinoma?
BCC is a locally invasive skin tumor. The main features are:
- Slowly growing license plate or nodule
- Skin color, pink or pigmented
- Their size varies from a few millimeters to several centimeters in diameter.
- Spontaneous bleeding or ulceration
BCC is very rarely life threatening. A small proportion of BCC grow rapidly, invade deeply and/or metastasis to local lymph nodes.
Types of basal cell carcinoma
There are several different clinical types of BCC, and more than 20 histological BCC growth patterns.
Nodular BCC
- The most common type of facial BCC
- Shiny or pearly nodule with a smooth surface
- It may have a central depression or ulceration, so its edges appear rolled up.
- Blood vessels cross its surface
- Cystic the variant is soft, with gelatinous content
- Micronodular, microcystic and infiltrative types are potentially aggressive subtypes
- Also known as nodulocystic carcinoma
Nodular basal cell carcinoma

Nodular basal cell carcinoma

Nodular basal cell carcinoma

Nodular basal cell carcinoma

Nodular basal cell carcinoma
superficial BCC
- Most common type in younger adults
- The most common type on the upper trunk and shoulders.
- Slightly scalyirregular plate
- Thin, translucent rolled edge
- Multiple microerosions
Superficial basal cell carcinoma

Basal cell carcinoma

Superficial basal cell carcinoma

Superficial basal cell carcinoma, face

Superficial basal cell carcinoma, back
Morphoeic BCC
- It is usually found in places in the middle of the face.
- Waxy, scar-like plate with indistinct edges
- Wide and deep subclinical extension
- May infiltrate cutaneous nerves (perineural spread)
- Also known as morpheo, morphoform or sclerosing BCC
Morphoid basal cell carcinoma

Morphoid basal cell carcinoma

Morphoid basal cell carcinoma

Morphoid basal cell carcinoma

Morphoid basal cell carcinoma
Basosquamous carcinoma
- Mixed basal cell carcinoma (BCC) and squamous cell carcinoma (SCC)
- Infiltrative growth pattern
- Potentially more aggressive than other forms of CCB
- Also known as basal squamous cell carcinoma and mixed basal squamous cell carcinoma
Basosquamous carcinoma

Basal cell carcinoma
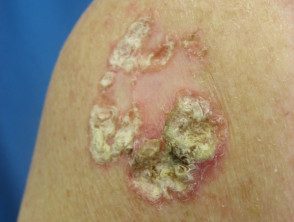
Basosquamous carcinoma

Basosquamous carcinoma
See more images of basal cell carcinoma.
- BCC affecting face images
- BCC affecting nose images
- BCC affecting eyelid images
- BCC affecting ear imaging
- BCC affecting trunk images
Complications of basal cell carcinoma
Recurrent BCC
Reappearance of BCC after initial treatment is not uncommon. Features of recurrent BCC often include:
- Incomplete excision or narrow margins at primary excision
- Morphoeic, micronodular and infiltrative subtypes
- Location on head and neck
Recurrent basal cell carcinoma

After PDT

After superficial surgery.

After fluorouracil

After imiquimod
advanced BCC
Advanced BCCs are large, often neglected tumors.
- They can be several centimeters in diameter
- They can infiltrate deep into the tissues under the skin.
- They are difficult or impossible to treat surgically.
Metastatic BCC
- Very rare
- The primary tumor is often large, neglected or recurrent, located in the head and neck, with an aggressive subtype
- May have had multiple prior treatments
- It can arise in a site exposed to ionizing radiation.
- It can be fatal
How is basal cell carcinoma diagnosed?
BCC is diagnosed clinically by the presence of slowly enlarging skin injury With typical appearance. The diagnosis and histological subtype are usually confirmed pathologically by a diagnosis biopsy or after the split.
Some typical superficial BCCs on the trunk and extremities are diagnosed clinically and have non-surgical treatment without histology.
What is the treatment for primary basal cell carcinoma?
Treatment for a BCC depends on its type, size and location, the number to be treated, patient factors, and the doctor's preference or experience. Most BCCs are treated surgically. Long-term follow-up is recommended to check for new lesions and recurrence; The latter may be unnecessary if histology has reported wide clear margins.
Excisional biopsy
Excision means that the lesion is cut and the skin is stitched.
- The most appropriate treatment for nodular, infiltrative and morphoid BCCs
- Should include a 3 to 5 mm margin of normal skin around the tumor
- Very large lesions may require a flap or skin graft to repair the defect.
- Pathologist will inform deeply and side margins
- Additional surgery is recommended for lesions that are incompletely removed
Micrographically controlled Mohs excision
Micrographically controlled Mohs surgery involves examining the carefully marked excised tissue under the microscope, layer by layer, to ensure complete excision.
- Very high cure rates achieved by trained Mohs surgeons
- It is used on high-risk areas of the face around the eyes, lips and nose.
- Suitable for ill-defined, morphic, infiltrative and recurrent subtypes.
- Large defects are repaired with a flap or skin graft
Superficial skin surgery.
Superficial skin surgery includes shaving, curettage and electrocautery. It is a quick technique using local anesthesia and does not require sutures.
- Suitable for little ones, well defined Nodular or superficial BCCs
- Lesions are generally located on the trunk or extremities.
- The wound is left open to heal by secondary intention.
- Moist wound dressings lead to healing within a few weeks.
- Possible variable scar quality
Cryotherapy
Cryotherapy is the treatment of a superficial skin lesion by freezing it, usually with liquid nitrogen.
- Suitable for small superficial BCCs in covered areas of trunk and extremities
- It is best avoided for BCCs in the head and neck, and distal on knees
- Double freeze-thaw technique
- It results in a blister that scabs over and heals in several weeks.
- Leaves a permanent white mark
Photodynamic therapy
Photodynamic therapy (PDT) refers to a technique in which the BCC is treated with a photosensitizing chemical and exposed to light several hours later.
- Current photosensitizers include aminolevulinic acid lotion and methyl aminolevulinate cream
- Suitable for small and superficial low-risk BCCs
- It is best to avoid it if the tumor is in the site with a high risk of recurrence
- Results in inflammatory maximum reaction 3 to 4 days after the procedure
- Repeat treatment 7 days after initial treatment
- Excellent cosmetic results.
Imiquimod cream
Imiquimod is an immune response modifier.
- Best used for superficial BCCs less than 2cm in diameter
- It is applied three to five times a week, for 6 to 16 weeks.
- Results in a variable inflammatory reaction, maximum after three weeks
- Minimal scarring is common.
Fluorouracil cream
5-Fluorouracil cream is a topical cytotoxic agent.
- Used to treat small superficial basal cell carcinomas
- Requires a long course, for example twice a day for 6 to 12 weeks.
- Causes inflammatory reaction
- Has high recurrence rates
Radiotherapy
Radiation therapy or x-ray treatment may be used to treat primary BCCs or as attached treatment if margins are incomplete.
- Mainly used if surgery is not appropriate
- It is best avoided in young patients and in genetic conditions that predispose to skin cancer
- The best cosmetic results achieved with multiple fractions
- Typically, the patient attends once a week for several weeks.
- Causes inflammatory reaction followed by scar
- Risk of radiodermatitis, late recurrence and new tumors.
What is the treatment for advanced or metastatic basal cell carcinoma?
Primary, recurrent, or locally advanced metastatic BCC requires multidisciplinary consultation. A combination of treatments is often used.
- Surgery
- Radiotherapy
- Targeted therapy
Targeted therapy refers to the hedgehog signaling pathway inhibitors vismodegib and sonidegib. These drugs have some major risks and side effects.
How can basal cell carcinoma be prevented?
The most important way to prevent BCC is to avoid sunburn. This is especially important in childhood and early life. Light-skinned people and those with a personal or family history of BCC should protect their skin from sun exposure every day, year-round, and throughout life.
- Staying indoors or in the shade in the middle of the day.
- Wear clothing that covers
- Generously apply broad-spectrum sunscreens with protection factor SPF50+ to exposed skin yes outside
- Avoid tanning indoors (hammocks, solaria)
Oral nicotinamide (vitamin B3) at a dose of 500 mg twice daily may reduce the number and severity of CCBs.
What is the prognosis for basal cell carcinoma?
Most BCCs are cured with treatment. Healing is more likely if treatment is carried out when the lesion is small.
About 50% of people with BCC develop a second one within 3 years of the first one. They also have a higher risk of other skin cancers, especially melanoma. Regular skin examinations and long-term annual skin checks by an experienced healthcare professional are recommended.


