What is the blue toe? syndrome?
Blue finger syndrome, also known as occlusive vasculopathy, It is a form of acute digital ischemia in which one or more toes turn blue or purple. There may also be scattered areas of petechiae or cyanosis of the soles of the feet.
Blue finger syndrome is associated with a small vessel. occlusion and it can happen without obvious precedent trauma or disorders that produce generalized cyanosis, such as hypoxemia or methemoglobinemia [1]. Most often it occurs in an older man who has had a vascular process.
Blue finger syndrome

Blue finger syndrome: ischemia

What causes blue finger syndrome?
The characteristic blue discoloration and pain in blue finger syndrome are caused by impaired blood flow to the tissue resulting in ischemia. Impaired blood flow is due to one or more of the following factors:
- Diminished arterial flow
- Damaged venous departure
- Abnormalities in circulating blood.
These are not mutually exclusive. For example, abnormal blood circulation can induce vasculitis and subsequent thrombosis of the arterioles and capillaries supplying blood to the toes, resulting in decreased arterial flow.
The causes of blue finger syndrome
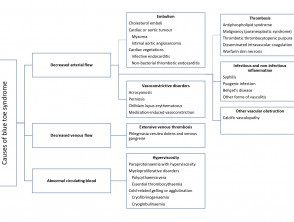
Adapted from Hirschmann JV, Raugi GJ. J Am Acad Dermatol 2009
Decreased arterial flow
Blockage or narrowing of the arteries by small clots that lead to blue finger syndrome can be the result of a number of different conditions.
Embolization
- Cholesterol the emboli are fragments of cholesterol or fibrin–platelet material released into the bloodstream by ulcerated arteriosclerotics plates in the large arteries (eg, the aorta, iliac and femoral arteries) and are the most common cause of blue finger syndrome. Risk factors include smoking, hypertension, elevated cholesterol levels and a recent angiogram or vascular surgery.
- Embolization (formation of a plunger, a floating mass in the bloodstream that can clog arteries) can also occur spontaneously [2].
- Plungers can originate from a heart tumor or from vegetations (clots or growths made of fibrin and blood platelets) of a cardiac myxoma or endocarditis (septic embolism). It is rare for an embolus to develop without any apparent cardiovascular risk factor or rushing event [3].
Thrombosis
- Thrombosis can form in the small vessels of the feet.
- May be the result of antiphospholipid syndrome, thromboangiitis obliterans, malignancythrombotic thrombocytopenic purple, disseminated intravascular coagulationand warfarin-induced skin necrosis [1].
Vasoconstrictor disorders
- Narrowing of blood vessels in the feet it can be the result of a contraction of the muscular wall.
- In Raynaud's disease, vasoconstriction tends to affect multiple fingers more severely than toes.
- Causes include drug-induced vasoconstriction (eg, a beta-blocker or an illicit drug such as cocaine) and / or acrocyanosis [1].
Infectious and non-infectious inflammation
The occlusion may also be due to syphilis, pyogenic infection (septicemia), Behçet's disease and other forms of vasculitis [1,4].
Other causes of vascular obstruction.
Narrow blood vessels may be due to calcified vascular disease (calciphylaxis) [5].
Impaired venous outlet
Abnormal venous drainage associated with extensive vein thrombosis produces phlegmasis cerulean dolens (a painful form of blue finger syndrome associated with the leg. edema) Many patients have predisposing factors for venous thrombosis, including:
- Immobility
- Clotting disorders
- The pregnancy
- Previous trauma to the leg
- Malignancy [6].
Abnormalities in circulating blood.
Blue finger syndrome may be due to abnormal blood constituents. Please refer to DermNet NZ page on skin conditions of hematological disorders
- Platelet tamponade
- Myeloproliferative disorders (eg, polycythemia rubra vera and essential thrombocythemia)
- Paraproteinemia (what causes hyperviscosity)
- Cryoglobulinemia
- Cryofibrinogenesis
- Cold agglutinin anemia
- Paroxysmal nocturnal hemoglobinuria [7]
What are the clinical features of blue finger syndrome?
The clinical features of blue finger syndrome can range from an isolated and painful blue finger to a diffuse multi-organ system disease that can mimic others systemic Diseases Any organ or tissue can be affected, although the skin and skeletal muscles of the lower extremities are almost always involved. [8].
Cutaneous abnormalities are generally one of the first symptoms; more commonly, blue or purple discoloration of affected fingers [9]. Discoloration can affect one foot or both, depending on the underlying pathophysiology. It is often painful and may be associated with claudication.
In a series of 223 patients with cholesterol embolization, the most frequent cutaneous findings were:
- Livedo reticularis or livedo racemosa (in the 49% of patients with cutaneous manifestations)
- Gangrene (35%)
-
Acrocianosis (28%)
- Ulceration (17%)
- Nodules (10%)
-
Purple (9%).
Livedo reticularis may be nopallor or paleness when discoloration disappears with pressure and / or fades with leg elevation [10]. Bleaching occurs in the early stages of blue finger syndrome, since the slow flow of desaturated blood results in temporary obstruction of blood flow [1].
- Pain in the affected blue toe or toes is usually acute onset and occurs at rest. Unbleached areas of the foot and distal the limb can also be painful [11].
- The affected toes are cold compared to the unaffected parts of the foot, which are warmer and look good.perfused [6]. The pulses of the foot may be normal.
- Peripheral foot pulses can be palpable If an occlusion occurs in the small arteries and arterioles instead of in the large palpable arteries [6].
What are the complications of blue finger syndrome?
Mild forms of blue finger syndrome have a good forecast and disappear without aftermath [one]. However, cholesterol fragments that block blood vessels to other organs can lead to a multi-organ disorder. [one]. Kidney involvement has a poor prognosis.
Patients with blue finger syndrome not treated by embolization may experience more emboli in the following weeks, resulting in substantial occlusion and ischemic waste of digits, the forefoot and the limb (dry gangrene), requiring amputation [6].
How is blue finger syndrome diagnosed?
Blue finger syndrome is a clinical diagnosis based on the patient's history and examination findings. Determining the underlying cause of blue finger syndrome is important to guide treatment. [one]. Usually there are clues to clinical evaluation, but to confirm the diagnosis, research in the form of laboratory blood tests, tissue biopsiesand radiological Images are required.
The story and exam should focus on:
- Hypertension or other risk factors for hypercholesterolemia and atherosclerotic diseases
- Fever (indicating cholesterol emboli, infective endocarditis, myxoma, thrombotic thrombocytopenic purpura and disseminated intravascular coagulation)
- Heart murmur (infective endocarditis and atrial myxoma)
-
Reticular livedo (cholesterol embolism, myxoma, antiphospholipid syndrome, hyperviscosity syndrome, cryofibrinogenesis, cryoglobulinemia, and calciphylaxis)
- Extensive edema in the ipsilateral leg (phlegm cerulean dolens)
- Hollenhorst plaques (cholesterol emboli) were seen on retinal examination
- Dilated veins, bleeding and exudates on retinal examination (hyperviscosity syndrome) [1–3].
A complete blood count that includes a white blood cell differential, erythrocytes sedimentation rate, and C-reactive protein can indicate elevated inflammatory Markers These are often nonspecific in blue finger syndrome and can occur with cholesterol emboli, as well as with many other inflammatory processes. Blood count and peripheral blood film can help diagnose bone marrow or autoimmune Liver diseases and renal Features must also be verified.
Other more specific blood tests may include:
- Coagulation tests for disseminated intravascular coagulation.
- Antinuclear antibodies
- Antiphospholipid antibodies
- Blood cultures (for suspected septic embolism)
- Hemolysis screen
- Cold agglutinins
- Cryofibrinogen level
- Cryoglobulin level
- Serum and protein in urine electrophoresis and immunofixation
- Hepatitis C (for suspected cryoglobulinemia)
-
Syphilis serology [1].
Images may include:
- A chest bone scan and / or thoracic and abdominal computed tomography or magnetic resonance image to search any aortic atheroma and underlying Cancer in associated malignant conditions
- Peripheral angiography and exploration of the limb arteries (to locate vessel narrowing, occlusion, and / or determine the source of emboli)
- Ultrasound of the abdomen and a venous duplex ultrasound scan to detect deep vein thrombosis
- A echocardiogram to detect cardiac tumors or vegetations due to endocarditis [1,12].
A definitive diagnosis is generally made by the histopathological confirmation of a biopsy of the affected skin or other involved tissues [13]. Biopsies in patients with poor peripheral vascular supply should be performed with caution as scarring is likely to be poor at the sampling site. Histopathological findings for cholesterol embolism show intravascular cholesterol crystals, which may be associated with macrophages, giant cellsand eosinophils [13].
What is the treatment for blue finger syndrome?
The principles of treatment revolve around addressing the cause of blue finger syndrome. This usually comes in the form of relief from occlusion and restoration of the continuity of arterial or venous vessels. [6].
- Medical anticoagulation (especially antiplatelet drugs) and endovascular or reconstructive surgical procedures are indicated for emboli and thrombosis, to remove the source of the clot, resolve occlusion, and restore blood flow.
- Hematologic treatment may be required when blue finger syndrome is due to hyperviscosity [14].
- Supportive and symptomatic treatments for blue toe syndrome include rest, warm conditions, appropriate dressings, and hydration. [14].
Address patient risk factors
Risk factors should be addressed in patients with advanced atherosclerotic disease, including:
- Of smoking cessation
- Control hypertension
- Serum cholesterol reduction.
Patients with stenotic Lesions must be followed carefully, as the progression of atheromatous disease will result in a high probability of recurrence of blue finger syndrome [6].

