What is gonorrhea?
Gonorrhea is a disease caused by infection with the bacteria Neisseria gonorrhoeae. Common sites of infection are mucous membranes of the urethra, endocervix, rectum, pharynx and conjunctiva. Gonorrhea is a sexually transmitted infection (STI). If the mother is infected, gonorrhea can also be transmitted to a newborn born vaginally. conjunctivitis.
Who is at risk for gonorrhea?
People at risk for gonorrhea are primarily sexually active people who come into contact with an infected person while not practicing safer sex.
Safe sex means using a condom or oral dam during sexual activity, which can include vaginal, oral, or anal contact.
What are the signs and symptoms of gonorrhea?
the incubation The average period is two to seven days.
Gonorrhea is asymptomatic in the 10-15% for men and even in the 80% for women.
The clinical characteristics of located Gonorrhea is different between men and women.
Men
- Pain when urinatingdysuria)
- Urethral download (often mucopurulent)
- Testicular discomfort and swelling due to epididymo-orchitis
- Anal discomfort and discharge due to proctitis)
Female
- Increased vaginal discharge
- Lower abdominal pain that may be due to the pelvis inflammatory disease (PID)
- Dysuria
- Sensitive periurethral glands and Bartholin glands
- Anal discomfort and discharge due to proctitis
Pharyngeal infection is becoming increasingly common, particularly in men who have sex with men (MSM) and is largely asymptomatic.
What is it disseminated gonococcal infection?
Complications of gonorrhea occur when the infection is not diagnosed or treated. This is more likely to occur when the infection is asymptomatic or when there is some barrier to accessing medical care.
Ascending infection in women
Ascending infection in women can cause pelvic inflammatory disease (endometritis, salpingitis, ovarian tubes). abscess) Scarring of the female upper genital tract can lead to chronic pelvic pain, ectopic pregnancy and infertility.
Ascending infection in men
Ascending infection in men can cause pain inflammation and swelling of the epididymis and testicles (epididymoorchitis).
pregnancy and neonatal infection
Gonococcal infection during pregnancy can cause miscarriage, premature birth, and postpartum endometritis. Vertical transmission from mother to child can cause neonatal conjunctivitis and, more rarely, bacterial septicemia.
conjunctival infection
Conjunctivitis in adults can occur by self-inoculation and is less common than neonatal conjunctivitis. Conjunctival gonococcal infection can cause scarring, permanent visual impairment, and blindness.
Disseminated gonococcal infection
Disseminated gonococcal infection results from the spread of the bacteria to the joints and other tissues. It occurs in 0.5-3% of infected individuals. A spectrum of symptoms includes:
- Tenosynovitis
- Skin lesions
- Polyarthralgia and oligoarthralgia, or purulent arthritis
- Constitutional symptoms (such as feverchills and discomfort)
Risk factors for disseminated gonococcal infection include recent menstruation, complement deficiencies systemic lupus erythematosus and microbial factors specific to some strains of the bacteria (for example, bacterial outer membrane porin B isoform 1 A).
Very rare complications of gonococcal infection include meningitis, endocarditis, osteomyelitis and vasculitis.
Which are the cutaneous manifestations of gonorrhea?
Although gonorrhea usually affects the mucous membrane surfaces, it can also affect the skin. A eruption It is present in the majority of patients with disseminated gonococcal infection. It affects the trunk, extremities, palms of the hands, and soles of the feet, and usually covers the face, scalp, and mouth.
Types injury include microabscesses, macules, papules, pustules and vesicles. Hemorrhagic injuries erythema knotty urticaria, and erythema multiforme occurs less frequently.
Gonococcal skin lesions.



How is the diagnosis of gonorrhea made?
The method used to detect gonorrhea depends on the setting and available resources.
Microscopy
Gram stain and visualization of gram-negative diplococci are appropriate in men with urethral discharge (sensitivity 90-95%) and are recommended in persons with rectal symptoms (see laboratory investigations for bacterial infections). They are not recommended in women (due to the low sensitivity of 20–50% in endocervical and urethral samples) or for pharyngeal samples.
Gonococcal Gram stain
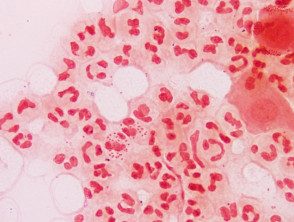
Gonococcus Gram stain
Culture
Culture involves collecting samples from appropriate sites (such as endocervical, urethral, rectal, and pharyngeal areas) and then inoculating onto agar plates that are selective for Neisseria gonorrhea. Neisseria gonorrhea requires special conditions (a CO2enriched environment) and rapid transport to a laboratory to ensure viability of the organisms. The advantage of culture is that it can provide antimicrobial susceptibility testing (which is important since this organism rapidly develops resistance to many antibiotics) and confirmatory tests.
Nucleic acid amplification tests
Nucleic acid amplification tests (NAAT) are increasingly available.
- For women, a vaginal or endocervical sample is equally sensitive.
- For men, first pass urine is preferred. Rectal and pharyngeal samples are considered based on sites of sexual contact.
- NAATs have high sensitivity and are often combined with one or two STI tests (eg, for chlamydia or trichomoniasis).
- Self-collection of samples is possible and results may be available sooner than with culture.
- NAATs do not routinely provide information on the sensitivity of gonococci to antibiotics.
What is the treatment for gonorrhea?
Treatment of uncomplicated gonorrhea should be started as soon as possible to avoid additional complications. The recommended empirical regimen for the treatment of Neisseria gonorrhea It is ceftriaxone 500 mg by intramuscular injection plus azithromycin 1 g orally. The addition of azithromycin is important as dual therapy is thought to limit the emerging resistance that begins to occur with ceftriaxone alone. Azithromycin will also treat a concurrent chlamydia infection.
Sexual activity should not take place until treatment is completed and all recent sexual contacts have been tested and treated appropriately.
If ascending infection is present, such as pelvic inflammatory disease or epididymoorchitis, treatment will require longer and more complex antibiotic regimens. It is important to check updated local guidelines.
Testing for other STIs should be performed in patients with gonorrhea to exclude coinfections.
How is gonorrhea prevented?
Reporting and treating recent sexual contacts and condom use are important to prevent reinfection of individuals and to help prevent the spread of gonorrhea in the population.

