What is amyloidosis?
Amyloidosis is the term used for a group of diseases in which one or more organs in the body accumulate various insoluble proteins (amyloid) in quantities to cause dysfunction of the organ system. Organs often affected include the heart, kidneys, gastrointestinal tract, nervous system and skin. Amyloidosis of the skin is called cutaneous amyloidosis. In this condition, amyloid or amyloid-like proteins are deposited in the dermis.
Types of amyloidosis
There are three major types of amyloidosis.
Primary amyloidosis
- Primary amyloidosis is a protein disorder. metabolism which originates in the bone marrow and is occasionally associated with multiple myeloma. It is also sometimes known as amyloid L (AL) chain type amyloidosis.
- Primary systemic Amyloidosis affects the heart, kidneys, liver, gastrointestinal tract, and central nervous system. Skin involvement occurs in approximately 30-40% of patients.
- Located Primary amyloidosis affects specific organs such as the skin (primary cutaneous amyloidosis), heart, eyes, respiratory tract, and bladder.
Types of primary localized cutaneous amyloidosis include:
- Lichen amyloidosis
- Macular amyloidosis
- Nodular amyloidosis
- Amyloidosis skin Dychromic.
Secondary systemic amyloidosis.
- Secondary systemic amyloidosis occurs as a complication of many chronic inflammatory diseases such as rheumatoid arthritis and osteomyelitis.
- It is also known as amyloid A (AA) amyloidosis and is the most common form of systemic amyloidosis worldwide.
- The kidney, liver and spleen are the organs most affected in secondary systemic amyloidosis. Skin involvement is rarely a feature of the disease.
Family (hereditary) amyloidosis
Familial amyloidosis is a rare form of amyloidosis that is inherited and most often causes cardiomyopathy and neuropathy in middle age The most common form, known as ATTR amyloidosis, is due to a mutation in transthyretin (TTR) gene in chromosome 5 and leads to defective hepatic transthyretin protein.
Clinical characteristics of primary amyloidosis.
Distinctive clinical features are found for each type of primary amyloidosis.
Systemic amyloidosis
Signs and symptoms of primary systemic amyloidosis are generally nonspecific and include:
- Fatigue
- Weightloss
- Edema
- Short of breath
- Daze
- Numbness, tingling sensation
- Hoarseness.
These can precede the diagnosis of amyloidosis by up to two years. However, when present along with the following specific symptoms, systemic amyloidosis should be considered a possible diagnosis.
- Carpal tunnel syndrome: Impaired function of the median nerve in the wrist as the nerve passes through the carpal tunnel.
- Skin lesions
- The most common skin findings are purple: petechiae (small red blood stains) and ecchymosis (small flat spots of blood that are round or irregular in shape and bluish/purple).
- Waxy papules, nodules or plates can be found around the eyelids, neck, groin and anogenital zone.
- Blisters filled with blood may form, for example by pinching the skin.
- the nail can be brittle and brittle (clove dystrophy)
- Patches hair a loss may arise (diffuse alopecia)
- Macroglossia: refers to an enlarged and firm tongue covered with blood spots, plaques and blisters.
- Edema (tissue inflammation) develops as a result of heart failure or nephrotic syndrome (kidney disease).
- Hepatomegaly (enlarged liver).
Systemic amyloidosis

Hereditary amyloid

Amyloidosis purpura

Amyloidosis purpura
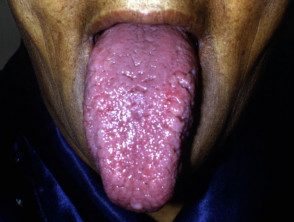
Macrogloassia due to systemic amyloidosis

Macrogloassia due to systemic amyloidosis

Macrogloassia due to systemic amyloidosis
Lichen amyloidosis
- Also called papular amyloidosis
- Lichen amyloidosis is the most common form of localized primary cutaneous amyloidosis.
- It presents as intense itching. eruption on the shins, thighs, feet and forearms.
- The lesions consist of multiple raised spots (papules) that are scaly and red/brown.
- The papules can get together in thickened plates.
- It appears to be more common in people of Chinese descent and men.
- It occurs most frequently in people between 50 and 60 years of age.
- It may be a variant of lichen simplex.
Lichen amyloidosis

Lichen amyloidosis

Lichen amyloidosis

Lichen amyloidosis
Macular amyloidosis
- In macular amyloidosis, lesions appear as flat dark brown or grayish spots that may join together to form patches of dark skin.
- The degree of itching varies from mild to severe.
- The lesions are usually distributed symmetrically over the upper back between the shoulder blades, on the chest, and sometimes on the arms.
- It appears to be more common in Asians, South Americans, and Eastern Orientals.
- It usually presents in early adult life and affects women more often than men.
Macular amyloidosis

Macular amyloidosis

Macular amyloidosis

Macular amyloidosis
Nodular primary localized cutaneous amyloidosis
- Also known as atrophic amyloidosis cutis nodularis and tumefactive amyloidosis
- Nodular primary localized cutaneous amyloidosis is the rarest form of primary localized cutaneous amyloidosis.
- Single or multiple firm nodules or plaques may appear on the trunk, extremities, extremities, face, and genitals.
- Nodular primary localized cutaneous amyloidosis usually has no symptoms and patients seek medical attention for its appearance.
- The nodules can be a few millimeters to a few centimeters and can be pinkish brown to red in color.
- The lesions tend not to ulcerate, but some may crack or split, particularly those on the soles of the feet.
Nodular amyloidosis

Nodular amyloidosis
Amyloidosis cutis dyschromicum
Amyloidosis skin Dyschromia is a recently described form of primary cutaneous amyloidosis that causes localization hyperpigmentation and hypopigmentation.
How is the diagnosis of amyloidosis made?
The diagnosis of the various types of primary cutaneous amyloidosis is made based on its clinical appearance and the characteristic histology changes observed in the skin biopsy. See also systemic amyloidosis. pathology.
What is the treatment of systemic amyloidosis?
Nonspecific treatment
Treatment is aimed at maintaining the function of the affected organs. For example, kidney failure can be treated with dialysis and congestive heart failure with diuretics.
Specific treatment
- Chemotherapy with melphalan and prednisone or dexamethasone (oral corticosteroids) may control systemic amyloidosis
- In secondary amyloidosis, colchicine may inhibit amyloid statement while the treatment is directed against the main cause.
- Managed monoclonal antibodies in use for systemic amyloidosis include lenalidomide and bortezomib.
- Bone marrow ablation can be carried out to eliminate the plasma cells and is followed by autologous stem cells transplant.
- Hereditary ATTR amyloidosis is treated with diflunisal or tafamidis (which stabilizes the abnormal transthyretin protein). Liver transplant is reserved for the most severely affected people.
Forecast
Most untreated patients die within 1 to 2 years after diagnosis of primary systemic amyloidosis due to heart or kidney failure.
What is the treatment of primary cutaneous amyloidosis?
Treatment of lichen and macular amyloidosis focuses on relieving itching. Sedative antihistamines may be moderately effective. Current and intralesional steroids may provide some relief if used with other treatments. Other treatments include topical dimethyl sulfoxide (DMSO) and phototherapy (UVB or PUVA).
Surgical treatment to remove amyloid deposits includes To be vaporization, dermabrasion and excision of individual injuries.
The primary goal of treatment for nodular primary localized cutaneous amyloidosis is to improve appearance. Various methods are used and include antibiotics, topical and intralesional corticosteroids, cryotherapy, dermabrasion, shaving, curettage and electrodesiccation, carbon dioxide laser and pulsed dye laser.
Primary cutaneous amyloidosis tends to persist or recur after treatment, but remains limited to the skin and does not progress to systemic disease.

